A hospital on high alert, days-long A&E waits and praise for hardworking staff - our day inside the NHSpublished at 17:59 GMT 13 February
 Sam Hancock
Sam Hancock
Live page editor
 Image source, PA Media
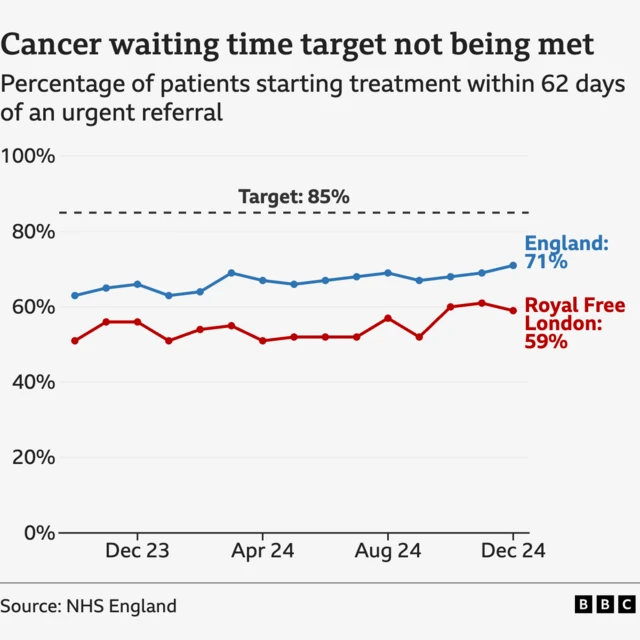
Image source, PA MediaAs the latest NHS England figures were released today, a team of BBC health reporters headed to the Royal Free Hospital in north London to see what happens in an NHS hospital on a day-to-day basis.
We spoke to Margaret, a pancreatic cancer patient, who said she was trying to "be positive" ahead of having surgery to remove a tumour. We spoke to a senior matron as the hospital began operating at its highest level of alert, treating patients in corridors. And we heard from a ward manager who explained the process of patients moving from A&E to wards, and the delays that occur due to a lack of beds.
Meanwhile, you - our readers - have been sharing your experiences with the NHS throughout the day and before we head off, we wanted to bring you a snapshot of what we've heard:
- Alan Cowling described having to spend four days in A&E - but said he couldn't "thank the hospital enough" for looking after him
- Lucy Russel recalled her experience in hospital following the birth of her daughter - saying her postnatal care was "emotionally traumatic"
- Trevor Hartnup said the older he got, the more "neglected" he felt by the NHS - recounting a recent hospital stay as "the worst experience in my 25 years as a patient"
- And Jane Paterson, telling us of her brother's "excellent care" in the days before his death, said "we've all had bad experience, but we forget to remember how bloody marvellous they [NHS staff] are!"
As our health editor Hugh Pym writes, research shows people are proud of the NHS - they just want it to do better.
We're going to bring our NHS live coverage to a close, but thank you for following along - and for contributing if you shared your stories with us. We're proud to have been able to tell them. For more updates on the BBC's day at the Royal Free, though, read our news story.