Goodbyepublished at 16:59 GMT 8 December 2022
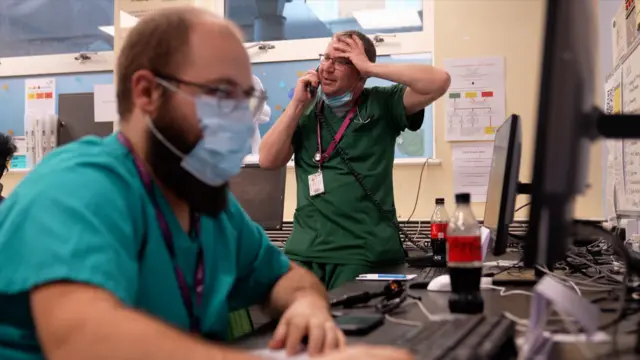
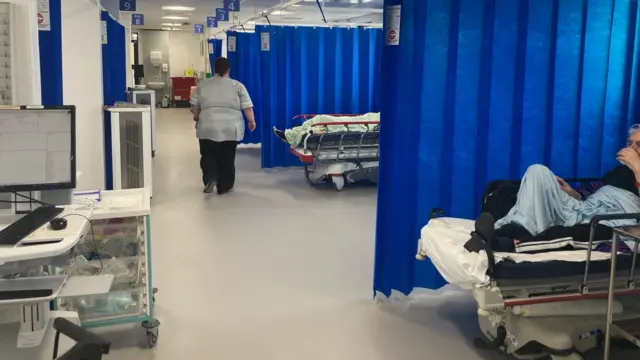
Thank you for joining us for our special day of coverage, reporting on the pressures faced by patients, doctors and nurses in the NHS.
The live page was brought to you by Sam Hancock, Gem O'Reilly, Laura Gozzi, Thomas Macintosh, Aiofe Walsh and Jo Couzens.
It was edited by Rob Corp, Philippa Roxby and Michelle Roberts.