What happened after the infections?published at 13:36 BST 20 May 2024
 Jim Reed
Jim Reed
Reporting from the inquiry
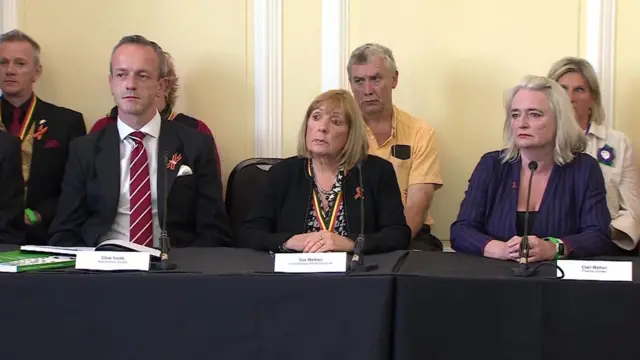
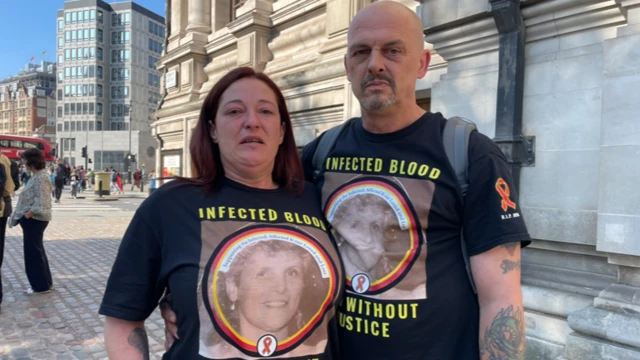
This inquiry has also been asked to investigate how victims of this scandal and their families were treated in the decades after they were infected.
Again it highlights a series of failures by government and the health authorities including:
- The absence of any meaningful apology and redress
- The “repeated use” of inaccurate, misleading and defensive lines which “cruelly told people that they had received the best treatment available”
- A “lack of openness, transparency and candour” from the NHS and government
- Long delays in providing support payments and a refusal to provide compensation
It also criticises the decision by successive governments to reject calls for a public inquiry by producing “flawed, incomplete and unfair” internal reports.
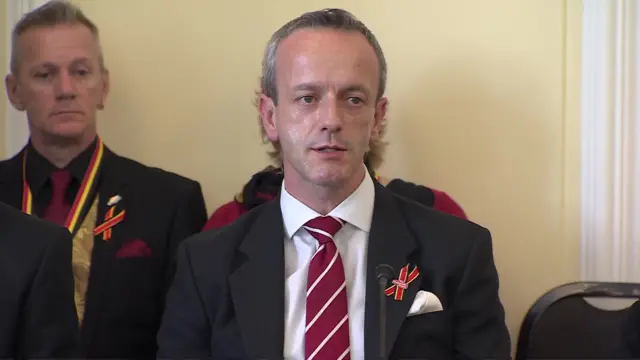
Sir Brian Langstaff, the chair of the inquiry, said it will be “astonishing to anyone who reads this report that these events could have happened in the UK”.
The families affected had been subjected to “a level of suffering which is difficult to comprehend, still less understand,” he adds, which was “compounded by the reaction of the government, NHS and other public bodies”.