The strange and curious history of lobotomy
- Published

It's 75 years since the first lobotomy was performed in the US, a procedure later described by one psychiatrist as "putting in a brain needle and stirring the works". So how did it come to be regarded as a miracle cure?
Deep in the archives of London's Wellcome Collection, that great treasure trove of medical curiosities, is a small white cardboard box.
Inside is a pair of medical devices. They are simple. Each consists of an 8cm steel spike, attached to a wooden handle.
"These two gruesome things are lobotomy instruments. Nothing sophisticated," says senior archivist Lesley Hall. "It's not rocket science is it?"
These spikes once represented the leading edge of psychiatric science. They were the operative tools in lobotomy, also known as leucotomy, an operation which was seen as a miracle cure for a range of mental illnesses.
For millennia, mankind had practised trepanning, drilling holes into skulls to release evil spirits.
The idea behind lobotomy was different. The Portuguese neurologist, Egas Moniz, believed that patients with obsessive behaviour were suffering from fixed circuits in the brain.
In 1935, in a Lisbon hospital, he believed he had found a solution. "I decided to sever the connecting fibres of the neurons in activity," he wrote in a monograph titled How I Came to Perform Frontal Leucotomy.
His original technique was adapted by others, but the basic idea remained the same.
Surgeons would drill a pair of holes into the skull, either at the side or top, and push a sharp instrument - a leucotome - into the brain.
The surgeon would sweep this from side to side, to cut the connections between the frontal lobes and the rest of the brain.
Moniz reported dramatic improvements for his first 20 patients. The operation was seized on with enthusiasm by the American neurologist Walter Freeman who became an evangelist for the procedure, performing the first lobotomy in the US in 1936, then spreading it across the globe.
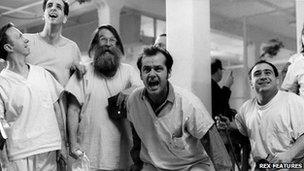
The hyperactive McMurphy, played by Jack Nicholson, is lobotomised in One Flew Over the Cuckoo's Nest
From the early 1940s, it began to be seen as a miracle cure here in the UK, where surgeons performed proportionately more lobotomies than even in the US.
Despite opposition from some doctors - especially psychoanalysts - it became a mainstream part of psychiatry with more than 1,000 operations a year in the UK at its peak. It was used to treat a range of illnesses, from schizophrenia to depression and compulsive disorders.
The reason for its popularity was simple - the alternative was worse.
"When I visited mental hospitals… you saw straitjackets, padded cells, and it was patently apparent that some of the patients were, I'm sorry to say, subjected to physical violence," recalls retired neurosurgeon Jason Brice.
The chance of a cure through lobotomy seemed preferable to the life sentence of incarceration in an institution.
"We hoped it would offer a way out," says Mr Brice. "We hoped it would help."
There were centres for lobotomy across the UK, in Dundee, North Wales and Bristol. But by far the most prolific lobotomist in the country, and indeed the world, was the neurosurgeon Sir Wylie McKissock, based at the Atkinson Morley hospital in Wimbledon.
"He was one of the great men of medicine of the 20th Century," says Terry Gould, who worked as McKissock's anaesthetist.
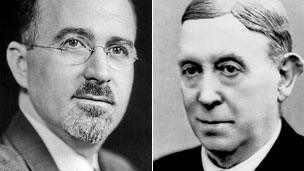
Freeman (left) built on Moniz's discovery
He believes his former boss performed around 3,000 lobotomies, as part of his famously speedy approach to surgery. "It was a five-minute procedure. Very quickly done," says Dr Gould.
As well as operating at Atkinson Morley, McKissock would travel across the south of England at weekends, performing extra leucotomies at smaller hospitals.
"He was quite prepared to travel down to whatever the hospital was on a Saturday morning and do three or four leucotomies and then drive away again," says Mr Brice.
He says the operation could have dramatic benefits for some patients, including one who was terrified of fire. "Funnily enough she finished up after I had done the operation very much better, but she went and bought herself a fish and chip shop with grossly hot oil in it."
However, he had increasing doubts about lobotomy, especially for patients with schizophrenia.
Psychiatrist Dr John Pippard followed up several hundred of McKissock's patients. He found that around a third benefited, a third were unaffected and a third were worse off afterwards.
Although he himself had authorised lobotomies, he later turned against the practice.
"I got increasingly conservative about it because I don't think any of us were ever really happy about putting in a brain needle and stirring the works," he says. "Not a nice thought."
In 1949, Egas Moniz won the Nobel Prize for inventing lobotomy, and the operation peaked in popularity around the same time.
But from the mid-1950s, it rapidly fell out of favour, partly because of poor results and partly because of the introduction of the first wave of effective psychiatric drugs.
Decades later, when working as a psychiatric nurse in a long-stay institution, Henry Marsh used to see former lobotomy patients.
"They had been lobectimised 30-40 years ago, they were chronic schizophrenics and they were often the ones were some of the most apathetic, slow, knocked-off patients," he says.
Mr Marsh, who is now one of Britain's most eminent neurosurgeons, says the operation was simply bad science. "It reflected very bad medicine, bad science, because it was clear the patients who were subjected to this procedure were never followed up properly.
"If you saw the patient after the operation they'd seem alright, they'd walk and talk and say thank you doctor," he observes. "The fact they were totally ruined as social human beings probably didn't count."