What's the evidence for the gluten-free lifestyle?
- Published

With food allergies on the rise we probably all know someone who has to avoid one foodstuff or another for medical reasons. Now, though, there is also the rise of the "gluten-free" lifestyle, removing most breads, pastas and cakes from the menu, writes Dr Chris van Tulleken.
It's estimated that 8.5 million people in the UK have now gone "gluten free" and it's a very fast-growing section of the supermarket with an expanding (and expensive) range of gluten-free alternative foods on sale. So, what's behind it all?
If you're one of those who sigh and tut at the perceived fussiness of the new gluten-free brigade, spare a thought for the 1% of the population who suffer from coeliac disease.

Find out more
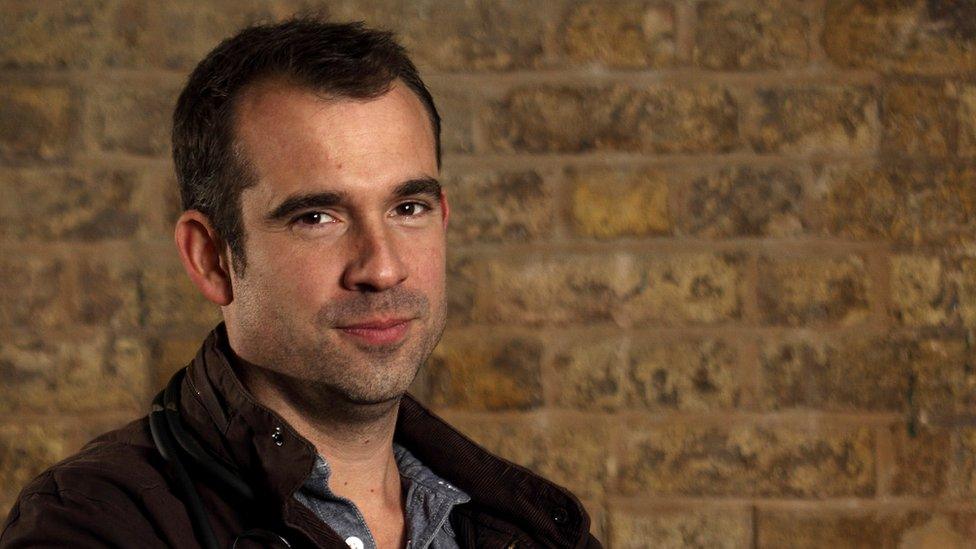
Chris van Tulleken presents Trust Me, I'm A Doctor which is on Thursday 8 September on BBC Two at 20:00 BST - catch up on BBC iPlayer

Coeliac sufferers have a lifelong autoimmune disease which means that gluten causes their immune system to turn on their own bodies, destroying the delicate linings of their guts and causing painful digestive symptoms as well as malnutrition and serious complications. The current boom in gluten-free products and gluten-awareness from restaurants is a huge benefit to them.
The vast majority of gluten-avoiders today, though, are doing it either as a diet to lose weight (not being able to eat most bread, pasta or cakes limits snacking options), or because they believe that avoiding gluten makes them feel better. What, then, is the evidence for that?
"Non-coeliac gluten sensitivity" is not a widely-recognised medical condition. Although many people who do not have coeliac disease claim to suffer gut symptoms like bloating and nausea when they eat gluten - and even other things like "brain fog" and tiredness - these have not been linked to any physiological changes that can be measured and hence used to make a clinical description and diagnosis.
The Trust Me, I'm a Doctor team signed up 60 (non-coeliac) volunteers willing to go gluten-free in the name of science. These included a good proportion of people who felt that they suffered symptoms when they ate gluten, and a good proportion of cynics, happy to go gluten-free in the hope of discovering that those who complained were merely hypochondriacs.

By performing the trial "double-blinded", we tried to stop either camp from being able to influence the results. That meant that although all 60 volunteers were asked to remove gluten entirely from their everyday diet, we provided them with a daily meal of pasta.
Most of the time this was gluten-free pasta, but we secretly slipped each of them gluten-containing pasta for two weeks within the trial period - but no one knew which two weeks each volunteer had been eating gluten, until the results were analysed. This meant that we could compare the volunteers' symptoms in the weeks they were eating gluten and the weeks they were gluten free and see whether they differed.
What, then, could we measure to try to determine whether some people really do suffer when they eat gluten?
Firstly, of course, there are the symptoms they felt - so we asked each volunteer to fill out a questionnaire each fortnight assessing the state of their gut and of their general health and wellbeing.
Then we wanted to measure any physiological markers that might indicate a cause for their symptoms.
Allergies are caused by a reaction in the immune system, specifically antibodies called IgE. Therefore, in order to check whether there might be any allergic reaction to gluten, we tested their IgE antibodies and other immune system markers every fortnight.

Intolerances, such as lactose intolerance, are quite different. Food intolerances are often due to a person not having the enzyme necessary to break down certain foodstuffs, although they may also be caused by substances in the foods themselves such as histamine content or additives.
A reaction because of intolerance is usually a slower onset than an allergy, sometimes taking hours or even days to manifest, and can lead to symptoms such as diarrhoea and bloating.
Many people feel that their problems with gluten are down to some kind of intolerance. These sort of gut symptoms usually cause some inflammation in the gut.
Recently Italian and American research groups claimed to have found biochemical markers of gut inflammation that were higher in people with "gluten sensitivity", when they ate gluten. We therefore measured three different markers of gut inflammation in our volunteers each fortnight.
So, how did our volunteers get on?
Well, they almost universally enjoyed the experiment. Many found it made them eat more healthily, lose weight and feel better. None of that, though, could definitively be ascribed to the lack of gluten in particular - it's possible we were just forcing them to consider what they ate more carefully.
Most, though, also felt that by the end of the experiment they could tell which weeks they were eating pasta containing gluten - overall, they reported significantly more gut symptoms in the fortnight that each was given gluten compared with the weeks when they were truly gluten-free.
As for the "health" symptoms such as tiredness and low mood, many did also report more adverse effects in the weeks they were being given gluten, but overall this was not statistically significant.
Admittedly it's difficult to find gluten-free pasta that is indistinguishable from "normal", and the Trust Me team had to have a few team dinners to road-test different options. The participants certainly couldn't have been sure which was which, but their guesses may well have influenced their self-reported symptoms.
What, then, of the objective blood test results? Well, here there were no significant differences between any of the markers we measured in the weeks they were having gluten and the weeks they were gluten free.
Nor were the levels of inflammatory markers higher in people who reported symptoms when eating gluten than those who didn't.

Bread was once absolutely central to the Western diet
So, does "non-coeliac gluten sensitivity" exist?
Well, many of our participants clearly thought so - but their guesses at which pasta contained gluten may have biased their opinions of their symptoms.
Our biochemical measures showed nothing at all - but that could mean that we were just measuring "the wrong things". The immune and inflammation systems are, after all, among the most complex aspects of the human body, and we have much yet left to understand.
On top of that, we are only just scratching the surface about understanding our relationship with our gut bacteria. There is the possibility that some people have gut bacteria that create symptoms when fed gluten-containing foods - something that might not have shown up in the markers we tested.
We, then, have found no test that could be used to diagnose "gluten intolerance" or "non-coeliac gluten sensitivity" and equally there is no evidence from any study anywhere to back up the use of popular home testing kits for "intolerances" - many expert groups around the world have spoken out against their marketing. Whatever they claim to measure, it hasn't been shown to be strongly linked with symptoms, so don't waste your money on them.
If you feel that you definitely suffer, then the advice is to first rule out coeliac disease. It is vital you continue to eat gluten before visiting your GP for this test, external.
Once coeliac disease and wheat allergy have been ruled out, the next step would be to try an "elimination diet", ideally under the supervision of your GP or trained practitioner. This involves cutting gluten out of your diet for at least two weeks and then reintroducing it - at the same time monitoring symptoms (and this is true of any food that you feel might be causing you problems). You may feel better simply because it makes you eat more carefully and healthily, but that's no bad thing.
It's important that if you are excluding foods from your diet that you do so under the supervision of your GP, a dietician or a trained practitioner. There is a danger when eliminating food groups that vital elements of nutrition are lost. This is especially important in growing children. Another concern is that without expert advice, you may end up eliminating particular food groups unnecessarily.
So, whether you are convinced non-coeliac gluten sensitivity exists, or think that the 6% of the population who claim to suffer from it are purely hypochondriacs, then the Trust Me, I'm a Doctor study will probably give you something to discuss over the dinner table with your friends - whilst you argue over the gluten content of the bread.
Chris van Tullekenpresents Trust Me, I'm A Doctor which is on Thursday 8 September on BBC Two at 20:00 BST
Follow @BBCNewsMagazine, external on Twitter and on Facebook, external