NHS front line: On the road with an ambulance crew
- Published

Karina Graham and Mandy Clark took the BBC alongside them on a 12-hour shift around Birmingham
As the NHS in England continues to struggle with low staffing and talk turns to potential strike action, the BBC joined two West Midlands paramedics for a day to see first-hand what life is like on the front line.
"I've come up against challenges that I've never had to face before as a paramedic," says Karina Graham, as she starts her 12-hour shift in Birmingham.
She's been in the job for eight years and says things have become much harder since the start of the pandemic.
"We're going to patients that have been waiting for far too long, having patients in the back of my ambulance that I know shouldn't be in the back of my ambulance, that need to be in hospital, knowing that it's detrimental to patients," she says.
Start of the shift: 09:30

Karina and fellow paramedic Mandy Clark log on for duty at the Hollymoor Hub in south-west Birmingham, and a job comes through straight away.
It's a category two call - the second most serious - which includes cases such as chest pain and strokes. The patient, 79-year-old Joyce, is struggling with her breathing.
Mandy and Karina do some checks that come back normal, but there's a build-up of fluid on Joyce's chest. They advise she goes to hospital for an X-ray.
They take her to Birmingham's Queen Elizabeth Hospital, a few miles out of the city centre, where six ambulances are queuing when they arrive. Because Joyce can go and sit in the A&E waiting room it means the ambulance doesn't have to hang on for a bed.
Mandy says this is fairly normal for this time of day, but it tends to get busier later.
"What we find is that we end up queuing in the afternoon," she says.
"Apparently, according to the statistics, hospital delays are slowing down."
But, she adds: "Working on the front line on the ground, I haven't noticed much of an improvement at all."
Karina says waiting can be "very frustrating".
"Sometimes we're sat there for 10, 12 hours and you can hear callouts and they're round the corner from where you are.
"And there's nothing you can do about it because you've got to stay with this patient."
So far this year, ambulances have spent more than a million hours waiting outside A&E to hand over patients, according to data from the Association of Ambulance Chief Executives.
This should happen within 15 minutes, but two-thirds of handovers took longer than this.
Every single day in September, nearly 400 patients and crews waited for more than three hours outside a hospital in England, the association says.
Four hours in: 13:20

The next job of the day is at a care home, where 96-year-old Gerda has fallen over and possibly broken her hip.
She fell at 09:20 and has been waiting for four hours by the time the ambulance arrives.
Her son Alan says she already faced a long wait in an ambulance outside a hospital a few months ago.
"We stood with the paramedics for 13 hours in the ambulance," Alan says. "And I think by the time she was seen it was something like 24, 25 hours".
Gerda is taken to the Heartlands Hospital, which has recently set up what's called a cohort area. It's a room, staffed by paramedics, where patients in beds can be dropped off so ambulance crews can get back on the road.
Karina and Mandy can leave Gerda pretty quickly to get back on the road, and West Midlands Ambulance Service told us the scheme was making a difference to handover delays.
For Mandy, jobs like this are what it's all about.
"So we've gone in, we've made her more comfortable, and then we've moved… to get treatment," she says. "And that's quite satisfying".
Karina estimates that only about 40% of their callouts are ones where people genuinely need an ambulance.
Six hours in: 15:30
A call comes through for a category one emergency, which is the highest priority.
The only details at first are the patient's age. He's a five-year-old-boy. And he's unconscious.
Guidelines state ambulances should arrive at these calls within seven minutes.
Mandy and Karina battle through the traffic, which is a nightmare.
"We don't drive like this for no reason," Karina says, as Mandy beeps the horn at a car pulling out in front of the ambulance.
At the scene, the situation is quite different from the information from the control room.
"We were presented with a four-year-old that was crying on the bed, so obviously no breathing difficulties," Mandy explains.
Karina and Mandy struggle to get information they need from mum because of a language barrier and, in the end, take the boy to hospital, to be checked over.
Afterwards, Mandy reflects that cases like this can be emotionally exhausting.
"Obviously we go to the job and we think it's one thing and then it's not," she says.
"So that's a quick flip. Sometimes you do need to decompress.
"But then unfortunately due to the demand it's - quick - and then we went on to the next one."
Eleven hours in: 20:00

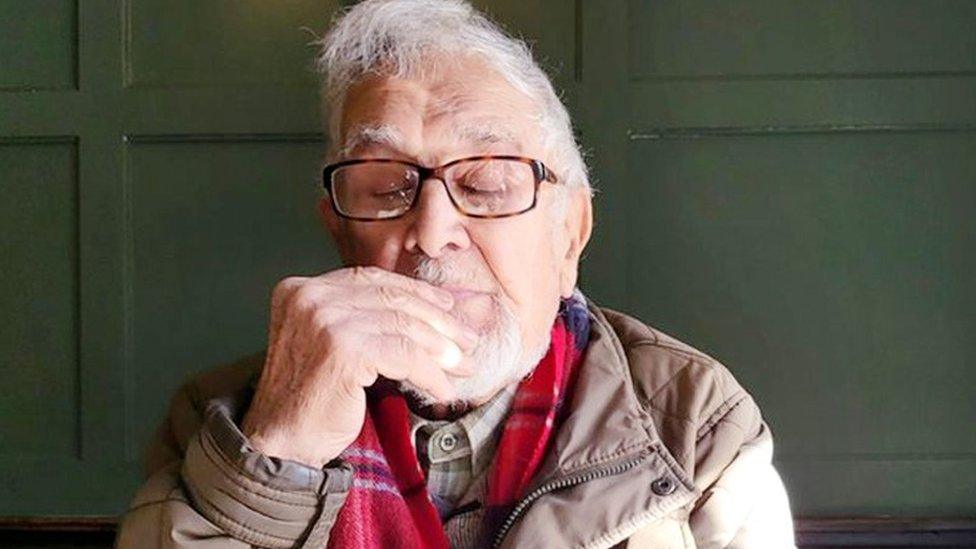
Birmingham's Queen Elizabeth Hospital - seen here in a file picture - is home to a busy A&E department
Mandy and Karina are on their last job of the day - another patient with chest pains.
They're back to the Queen Elizabeth Hospital, where there are, like before, six ambulances waiting.
There haven't been any major delays with the service they've provided today and Karina says she wishes this was always the case.
She tries to remember if there's ever been a time when she's got there too late due to handover delays.
"I can't say for 100% if I've thought 'would that patient have died if they were delayed or not?'," she says.
"But I would say that I've definitely gone to patients where there's been a detrimental effect on them waiting for us to get there."
The government says the health secretary is committed to easing pressures on the ambulance service by discharging more patients from hospitals, increasing the number of 999 call handlers and creating more beds.
But what does Karina think the solution is?
"Well, today has been really positive…maybe these cohorts that are being staffed by paramedics."
She says she was initially very sceptical about the scheme.
"I was like: 'Why are paramedics coming off the road to sort out a hospital's problem?'," she says. "But actually what it's done is resolved the ambulance's issue."
"If they can continue to work together and get the patients in and free us up to carry on and get out to the patients and do the job that's all I really care about.
"So if that works, fantastic."
You can listen to the full episode of File on 4's 'Is the patient breathing?' on BBC Sounds.

Follow Newsbeat on Instagram, external, Facebook, external, Twitter, external and YouTube, external.
Listen to Newsbeat live at 12:45 and 17:45 weekdays - or listen back here.
Related topics
- Published25 July 2022

- Published14 October 2022

- Published13 October 2022

- Published16 June 2022