Antibiotic-resistant superbug evolved on hedgehogs
- Published

The research has revealed how natural processes can give rise to antibiotic resistance, but hedgehogs are not the source of most human MRSA infections
An antibiotic-resistant superbug - a type of MRSA - evolved naturally as a result of a battle between a fungus and bacteria on the skin of wild hedgehogs.
The evidently "hedgehog-derived" bacteria developed in nature long before the antibiotics we are familiar with were discovered.
An international research team found that a skin fungus common in hedgehogs naturally produces antibiotics.
Bacteria on the animals' skin developed antibiotic resistance in response.
The researchers say their findings, published in the journal Nature,, external shows how natural biological processes - not antibiotic use - drove the emergence of this particular superbug about 200 years ago.
The specific bacterium, called mecC-MRSA, was first found in dairy cattle and it had been assumed that the use of antibiotics on dairy farms had caused it to develop its resistance.
This is, though, just one, relatively rare example of antibiotic resistance arising naturally. And the discovery "represents a tiny fraction of the risks compared to overuse of antibiotics in a human medical context", one of the lead researchers, Prof Mark Holmes from the University of Cambridge, told BBC News.
MecC-MRSA causes about one in 200 human MRSA infections. The overuse of antibiotics, both in humans and farm animals, continues to drive the emergence of other, resistant, disease-causing strains.
The study itself has solved a long-standing mystery about the source of this particular type of MRSA, which veterinary scientists from the University of Cambridge discovered a decade ago.
"We tried to work out how much of a problem it was - so we looked in wildlife and in farm animals and found that it was clearly very widely distributed in nature," explained Prof Holmes. "When we looked at hedgehogs in particular, about half of the animals we sampled had this type of MRSA."
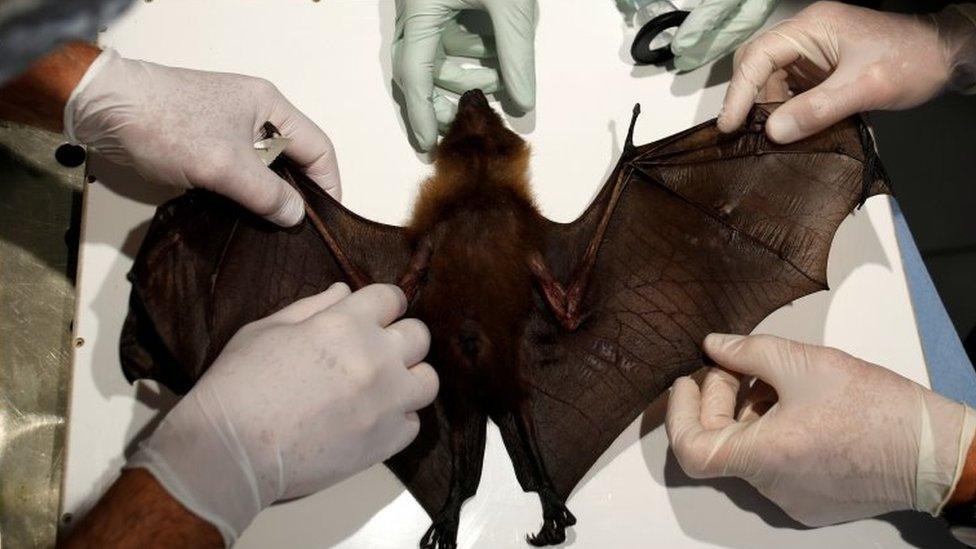
Teaming up with biologists, wildlife researchers and with hedgehog rescue centres all around Europe, the scientists then focused their investigations on hedgehogs

The fungus (in the centre of the petri dish) produces antibiotics, which kill methicillin-susceptible Staphylococcus aureus bacteria but not MRSA, resulting in a clear zone on the right
"We wanted to know," Prof Holmes explained, "what's so special about a hedgehog that means there's a lot of these resistant bacteria?"
Research colleagues at the Statens Serum Institut in Copenhagen, Denmark, studied more than 1,000 samples of bacteria taken from wildlife around Europe. They built a genetic code-based timeline , which revealed that the resistant strain had emerged in European hedgehogs in the early 1800s - long before the clinical use of antibiotics.
"The fungus growing on the hedgehog was releasing penicillins," explained Prof Holmes.
"The bacteria needed to be resistant because, if you want to live on the hedgehog - where there's a fungus, you have to be resistant to the antibiotics it's producing."
Prof Holmes added that the risk to human health from this type of MRSA was "very tiny - almost insignificant".

Don't fear the hedgehog: The animals have carried the bacteria for two centuries and caused no major infections in humans
Hedgehog expert and co-author of the study, Dr Sophie Lund Rasmussen from the University of Oxford explained: "Hedgehogs have carried this bacterium for at least 200 years without causing any major infections in humans.
"So the advice is [still] to appreciate and support the hedgehogs entering your garden and to maintain a good hand hygiene when feeding and possibly handling hedgehogs. Both for the sake of the hedgehogs and ourselves."
Hedgehog penicillin
The evolutionary "arms race" on the hedgehog's skin is a natural example of what Alexander Fleming saw on his petri dish when he discovered penicillin in 1928 - he noticed that no bacteria could survive close to a mould - a fungus - that had contaminated the gel in his dish.

Antibiotic resistance: A silent pandemic
Antibiotic resistance is one of the biggest threats to global health, food security, and development today
Antibiotic resistance occurs naturally, but misuse of antibiotics in humans and animals is accelerating the process
A growing number of infections - such as pneumonia, tuberculosis, gonorrhoea, and salmonellosis - are becoming harder to treat as the antibiotics used to treat them become less effective.

The study is part of an ongoing effort by these scientists to understand where "reservoirs" of antibiotic resistant bacteria are, how they emerge and what practices and sources pose the greatest risk to people.
"The reassuring thing is to be reasonably confident that it isn't the overuse of antibiotics in dairy farms that leads to this type of MRSA being present in people," said Prof Holmes. "But that does not mean that we should relax [the rules] on the use of antibiotics.
"It isn't just hedgehogs that harbour antibiotic-resistant bacteria - all wildlife carries many different types of bacteria, as well as parasites, fungi and viruses," he added.
"Wild animals, livestock and humans are all interconnected: we all share one ecosystem. It isn't possible to understand the evolution of antibiotic resistance unless you look at the whole system."
Follow Victoria on Twitter, external
Related topics
- Published17 November 2021

- Published6 July 2020