Experimental drug for Ebola patient Pauline Cafferkey
- Published

Pauline Cafferkey is an associate public health nurse at Blantyre Health Centre, South Lanarkshire
Ebola patient Pauline Cafferkey is receiving an experimental anti-viral drug and blood from survivors of the disease, doctors in London have said.
Specialists at the Royal Free Hospital in Hampstead, where the nurse is being treated, did not name the drug.
Dr Michael Jacobs said Ms Cafferkey was in isolation and was sitting up in bed, talking and reading.
As the disease has no known cure and is unpredictable, Dr Jacobs said they would know more in a week's time.
He said Ms Cafferkey had agreed to all the treatments and her family had been to see her.
"She's a nurse, a fellow professional, so we have been able to discuss things in great detail," he said.
Dr Mike Jacobs, infectious diseases specialist, confirmed Ms Cafferkey was receiving plasma and an unnamed experimental drug
"She's as well as we can hope for at this stage of the illness. She's had the treatment, it's gone very smoothly, no side-effects at all."
The drug and the convalescent plasma are part of a tranche of experimental treatments, he said.
"We simply don't know what the best treatment strategies are," he added.


Analysis
By James Gallagher, Health editor, BBC News website
This is a difficult time for doctors. Potential Ebola drugs exist yet there is hardly a scrap of evidence that any of them work.
Two of the most promising are brincidofovir and favipiravir.
Tests in tissue samples suggest the anti-virals have the potential to stop Ebola replicating once it infects cells.
Brincidofovir has been tried on some patients in the US and both drugs have entered clinical trials in West Africa.
However, the results are not expected until February.
The effectiveness of using the blood of survivors is equally uncertain until the results of trials come through.
Ebola therapies and vaccines are now being tested at unprecedented speed during this outbreak.
But for patients infected today, doctors simply do not know if these experimental options will make a difference.

Ms Cafferkey, a public health nurse at Blantyre Health Centre in South Lanarkshire, is receiving treatment via a quarantine tent after returning to Glasgow from Sierra Leone on Sunday.
She was working in the West African country as part of a Save the Children team. She travelled home via Casablanca, Morocco, and London's Heathrow Airport.
Ms Cafferkey was screened for the disease at Heathrow and told officials she believed a fever might be developing.
Her temperature was taken seven times in total and was normal each time, so she was allowed to fly home to Scotland.
She was placed in an isolation unit at Gartnavel Hospital in Glasgow after becoming feverish on Monday.
Ms Cafferkey was transferred by RAF Hercules plane to London and on to the Royal Free's specialist treatment centre on Tuesday.

Ms Cafferkey had travelled from Freetown in Sierra Leone via Casablanca
Ebola is transmitted by direct contact with the bodily fluids of an infected person, such as blood, vomit or faeces.
The virus has killed more than 7,800 people, mostly in West Africa, since it broke out a year ago.
The World Health Organization says the number of people infected by the disease in Sierra Leone, Liberia and Guinea has now passed 20,000.
Screening protocols
Ms Cafferkey's case has raised questions about the screening process in place for passengers leaving West Africa and arriving at Heathrow.
The chief medical officer for England, Dame Sally Davies, said Ms Cafferkey had been in the early phase of the disease when she made the journey back to the UK and her fellow passengers were at "very low risk" of being infected.
She told the BBC: "The public health risk is negligible - Ebola's very difficult to catch."
While the correct protocols had been followed, she said, the precautions were always under review.
A Department of Health spokesman said it would review the screening protocols.

Temperature screening
A normal body temperature is considered 37C
A raised temperature is one sign of Ebola and forms a core part of entry screening
The UK uses a relatively tough 37.5C as the cut off for further testing
Belgium and Australia use a higher threshold of 38C
India uses 38.3C
Spain and the US use 38.6C

Prof Andrew Easton, a virologist from University of Warwick, said it was difficult to detect the early stages of the virus but the questions asked during the screening process needed to be looked at.
"There has to be some kind of question asked about quite how those questions were posed to the nurse, what the responses were and then how things moved on from there," he told the BBC.
But British doctor Oliver Johnson, who has been based in Sierra Leone and was on the same flight as Ms Cafferkey, warned against imposing stricter screening measures.
"Unless we have evidence that there have been further transmissions or infections, I think the biggest mistake to make right now would be to try and change a system that appears to be working in a way that makes it more difficult to respond in West Africa to end this outbreak," he said.
Ms Cafferkey is the second UK case of Ebola. Another nurse - William Pooley - recovered from Ebola in September after also being treated at the Royal Free Hospital.
He donated some blood plasma and was treated with the anti-viral drug ZMapp, of which there are no stocks left.
Dr Jacobs said the cases "were quite separate from one another".
"We're starting from the beginning again," he said. "We're treating Pauline absolutely on her own merits."
He said there was "a European pool" of recovered patients' blood plasma and they had identified "the best plasma for her".
It is hoped the antibodies in the plasma will help her immune system fight the disease.

What are the symptoms?
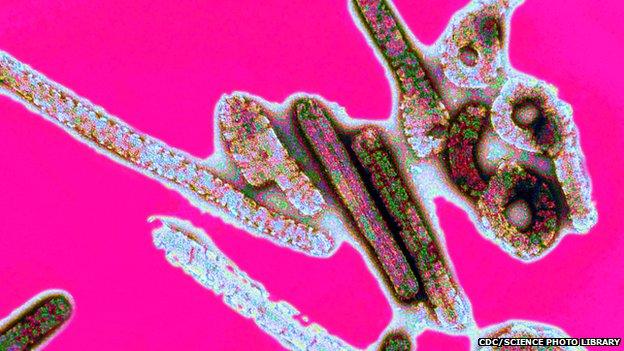
The Ebola virus causes a range of painful and debilitating symptoms
The early symptoms are a sudden fever, muscle pain, fatigue, headache and sore throat.
This is followed by vomiting, diarrhoea, a rash and bleeding - both internal and external - which can be seen in the gums, eyes, nose and in the stools.
Patients tend to die from dehydration and multiple organ failure.
