Payout after woman was kept alive against her will
- Published
Woman was kept alive despite her advance directive wishes
The family of an 81-year-old woman has received a £45,000 payout after she was kept alive against her will.
Brenda Grant made a living will stating she feared degradation and indignity more than death after seeing her mum lose independence through dementia.
But the George Eliot hospital, in Nuneaton, Warwickshire, misplaced the document and she was artificially fed for 22 months.
The trust has apologised for its failure.
Mrs Grant, from Nuneaton, had an advance directive drawn up to say if she were no longer of sound mind or had suffered from a list of medical ailments, she should not have treatment to prolong her life.
It also confirmed she should not be given food, but that distressing symptoms should be controlled by pain relief even though the treatment might shorten her life.

Mrs Grant's daughter said she wanted to prevent other people going through similar problems
In October 2012, Mrs Grant suffered a catastrophic stroke that left her unable to walk, talk or swallow.
After spending nearly three months in the George Eliot Hospital she was fitted with a stomach peg so she could be fed directly, then discharged into a nursing home.
The hospital had the advance directive but it was hidden in the middle of a thick pile of medical notes, Mrs Grant's daughter Tracy Barker said.
Once in the nursing home, Mrs Grant became agitated and tried to pull out the tubes in her arm, prompting staff to put mittens on her hands.
Mrs Barker said: "She had a fear of being kept alive because she had a fear of going into a nursing home.
"She never wanted to be a burden to anybody, so she wouldn't have wanted any of us to look after her."

Brenda Grant, pictured with her grandson, "never wanted to become a burden to anybody"
Mrs Grant did not tell her children about the living will.
It was her GP who alerted them to it shortly before Mrs Grant was re-admitted to hospital.
In a meeting with hospital medics, the GP then argued alongside Mrs Grant's family that her living will should be respected, Mrs Barker said.
Tubes were withdrawn and she died a few days later on 4 August 2014.

What is a living will?
A living will, or advance decision, is a document that sets out a person's wishes regarding health care and how they want to be treated if they become seriously ill and unable to make their own choices
The document allows people to refuse treatment, even if it might lead to death, and is legally binding
Some advantages are that they help medics and relatives take difficult decisions, but it can also be difficult for a healthy person to fully imagine what they would really want in those situations
To arrange one, legal advice is recommended while discussing the matter with a healthcare professional who knows your medical history. The outcome should then be shared with all those involved in your care
To refuse potentially life-sustaining treatment, the document must be signed and witnessed and include the statement "even if life is at risk as a result"
Sources: Age UK and BBC

"I'm very, very angry with myself that I let my mum suffer for two years that she didn't need to suffer for," Mrs Barker said.
"I didn't want my mum to die, nobody wants their mum to die.
"But my mum died the day she had that stroke because she was never, ever capable of doing anything that she did before.
"I know she would not have wanted to live like she was."
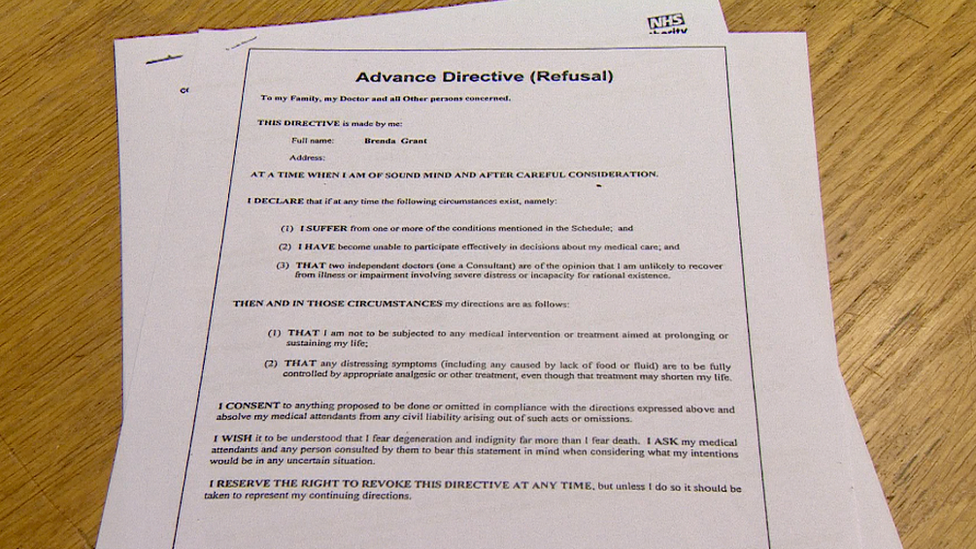
Brenda Grant's advance directive was buried in the middle of a thick pile of medical notes, her daughter said
Mrs Barker said she had sought legal advice to highlight the case so the same thing did not happen to others.
Richard Stanford, from law firm BTTJ, said: "It was a really interesting case, we instructed a human rights barrister very early on because the case appeared to be unique."
The George Eliot Hospital Trust admitted liability and in an out-of-court settlement agreed to pay £45,000.
In a letter, it stated: "It is accepted that the trust failed to act in accordance with the deceased's advance directive and failed to store the advance directive in a way that it could easily be noted."
The trust said it had now begun recording the existence of an advanced directive on the front page of a patient's notes.
- Published21 September 2017

- Published29 July 2017
- Published21 December 2016

- Published23 September 2016
