What lies behind the rise of the contraception app?
- Published

The NHS said the natural fertility awareness method, if followed consistently and correctly, could be up to 99% effective
The contraceptive pill was celebrated for the control and freedom it gave women when it first became available in the 1960s. Since then, most women in the UK have used hormone contraception at some stage of their lives. So why are some now turning to technology instead?
Montana Brown - known for her appearance on the ITV show Love Island - recently announced she was pregnant, two years after coming off hormone contraception.
In a post on her Instagram page, the influencer said she had been tracking her cycle naturally, a form of contraception called the natural fertility awareness method.
"It's taught me so much about my cycle that when the time came to make the switch and plan for a baby, I felt so in tune with my body," she wrote.
The post was part of a paid advert with Natural Cycles - an app established in 2013 that now has 2.5 million registered users.
In 2018 Natural Cycles became the first birth control app to be cleared by the US Food and Drug Administration., external
Its makers said it used an algorithm to determine a woman's fertility status based on body temperature and has claimed a 93% success rate - the same as the contraceptive pill in normal use.
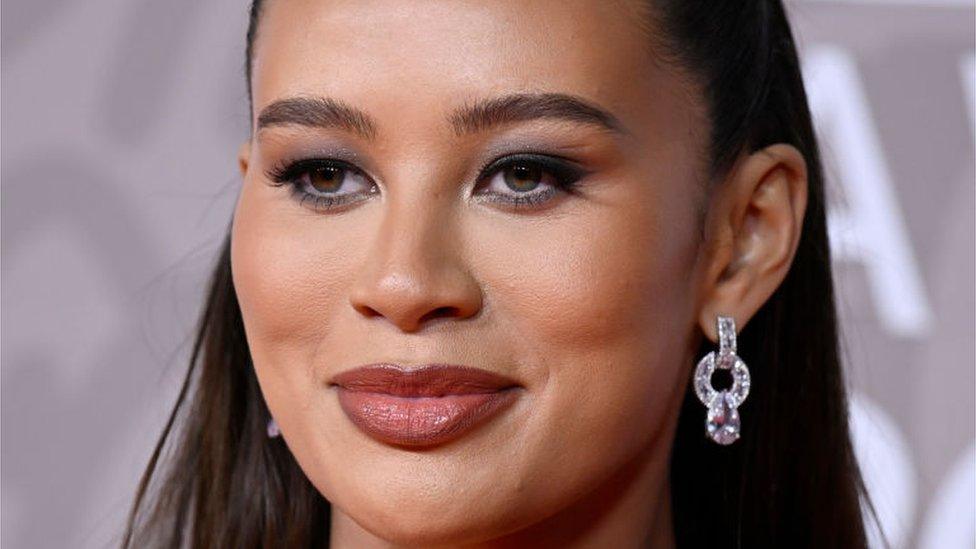
Montana Brown recently announced she was pregnant
The idea behind fertility apps is that they offer an alternative to traditional forms of contraception, and they work by highlighting the days when they calculate that pregnancy is most likely to occur. These depend on an individual's menstrual cycle.
However, there have been complaints about Natural Cycles from women who say they became pregnant while using it.
A Natural Cycles spokesperson said: "As with any contraceptive, it's important the product is used correctly to maximise effectiveness - as no method is 100% effective in preventing pregnancy, even when used perfectly."
She added the app's effectiveness was "higher than most fertility awareness methods".
The NHS stresses that condoms are the only type of contraception that can both prevent pregnancy and protect against sexually transmitted infections (STIs).
In 2018, a Facebook advert for the app was banned by the UK's Advertising Standards Authority, with claims that it was "highly accurate" and "provided a clinically tested alternative to other birth control methods" found to be misleading.
Despite this, the app claims to have hundreds of thousands of users in the UK, while other fertility tracking apps - like Flo and Clue - also claim to have millions of users worldwide.
So what is behind the rise of technology contraception?

'There's a risk in everything'

April has spent the last 10 years tracking her body temperature for contraception
April Inskip, from Leicestershire, has been using the natural fertility awareness method for almost a decade.
Over the course of eight years she tried different hormonal contraceptives before deciding they were not right for her.
"As I got older I realised it simply wasn't worth the toll [the pill] took on my body.
"I felt lethargic, moody, my skin frequently broke out randomly and I didn't want to mess any further with my hormones," she said.
April takes her basal body temperature first thing in the morning and records her reading in an app on her phone.
Her daily readings are plotted on to a virtual chart that allows her to see the relevant peaks or dips throughout her cycle.
"I prefer to see the whole chart rather than have an app take the information and interpret it for you," she said.
"I am very confident in reading my body and comfortable with this method."
April said that if she did fall pregnant she would not feel any different to how she would feel if she was on another form on contraception and it failed.
"I wouldn't blame the method, as there is a risk in everything," she said.
"If you have any doubts and are charting to avoid pregnancy then you just use a barrier method as back-up. That being said, even condoms aren't 100% effective."
According to the NHS, minor side effects of the pill can include mood swings, nausea, breast tenderness and headaches.
It said there was a very low risk of serious side effects, such as blood clots and cervical cancer.

'It has helped me understand my body'

Helen said it took two years for her periods to return after coming off the mini pill
Helen, from Nottinghamshire, has been following the natural fertility awareness method since stopping hormone contraception three years ago at the age of 30.
She said she had taken the mini pill for several years but felt it was affecting her mood.
"It gave me the idea to try coming off hormonal contraceptives altogether to see if there was any change," she said.
"I felt so much better in myself; however it did take two years for my periods to return."
Helen, now 33, said she does not plan to have children in the near future but believed she was "mature enough and financially stable enough" to cope if she did become pregnant.
She said: "I am so glad that I stopped taking hormonal contraception before I actively wanted children, as I was not equipped with the knowledge that it might take so long for my body to return to normal."
She tracks her cycle with the help of an app on her phone.
"I've learned more about my cycle and my body from this app," she said.
"It has helped me understand the changes to expect in my body over the month: what is normal, what is potentially abnormal."

'I listen to my body'

Laura said she felt a lot more comfortable using the natural fertility awareness method
Laura, from Derbyshire, said she was avoiding returning to hormone contraception until she had finished growing her family.
She gave birth to her first child in 2021 - later than she had been planning.
"It took us nearly a year and a half to actually conceive, which I do believe is partially due to the amount of time I was on the pill for," she said.
Laura, 33, had been on the combined pill from the age of 17 to 29.
She had a six-month break when she was 21 and during that time her period did not return.
"At the time I was so young, I wasn't really thinking about children so I really didn't think about the impact the pill was having on my body," she said.
Laura said she was not planning to get pregnant again for a while and was following the natural fertility awareness method to control this.
She also used an app on her phone to help but did not depend entirely on technology.
"I listen to my body a lot more and, as long as you're tracking where you are in your cycle, you should be able to figure out what stage you're at," she said.
"I'm a lot more comfortable than I ever have been on any medication.
"I do feel a lot more in tune with my body now than I ever have been."
Laura said if this method failed and she did get pregnant sooner that she wanted to, it would not be an unwanted pregnancy.
"Whilst we're not quite ready for baby number two, children are a blessing so we would be happy that we've been able to conceive again," she said.
The NHS said it could take a while for women's periods to come back after they stopped taking the pill and, when they did return, they could be irregular.
This was because the pill contains hormones that stop ovulation each month.
It said women should allow up to three months for their natural menstrual cycle to fully re-establish itself.
"It's unlikely the time you've been on the pill will cause infertility," NHS advice says, external.
"You might be able to conceive immediately after you stop taking it.
"However, while the pill does not cause fertility problems, it can mask underlying problems you may already have, such as irregular periods."

'Not suitable for everyone'

Annabel Sowemimo said the natural fertility awareness method was not suitable for everyone
According to the NHS, the natural fertility awareness method involves identifying the signs and symptoms of fertility during the menstrual cycle.
These include the length of the cycle, daily body temperature readings and changes to cervical secretions.
It said if followed consistently and correctly, it could be up to 99% effective.
However, Annabel Sowemimo, a doctor from the Leicester Sexual Health NHS service, said it was not suitable for everyone.
"If your lifestyle isn't stable, if you're not in the same place and you're not going to have access to your calendar, your thermometer, if your sleep pattern is irregular, all of these things can make it difficult and reduce the reliability of the method," she said.
Dr Sowemimo said it would also not be recommended to women with irregular cycles, polycystic ovary syndrome (PCOS), or women that were postpartum.

Dr Annabel Sowemimo said evidence did not support the view that long-term use of hormone contraception could cause infertility
Dr Sowemimo said she had other concerns about technology being used for the natural fertility awareness method.
"The issue with some of the apps that we see, they're subscription based, so they are a full-profit method of contraception," she said.
"They have the benefit of inflating or making it seem more effective than it is.
"Some of the developments we see also, they have real potential, but they are going to market far too soon before they have a reliable evidence base.
"That's because there's a lot of pressure from investors."
Dr Sowemimo said social media had played a role in influencing some women not to use hormone contraception.
"With the rise of TikTok, people are sharing information that is making people a bit more wary of contraception side effects so it is a trend that is very clear," she said.
She said the suggestion that long-term use of hormone contraception could cause infertility was not correct.
"People are fearful, particularly because we are having kids later and later," she said.
"The bigger impact is likely people's dwindling fertility in your late-to-mid 30s, rather than the impact of contraception on your fertility."

Follow BBC East Midlands on Facebook, external, on Twitter, external, or on Instagram, external. Send your story ideas to eastmidsnews@bbc.co.uk, external.
Related topics
- Published8 December 2022

- Published9 February 2017

- Published4 December 2011
