Cost of living: Health of London's poorest hit hardest
- Published

It is feared health and wealth divides in London are deepening (stock photograph)
The Covid-19 pandemic revealed some stark health and wealth inequalities throughout London's communities, with the poorest hit the hardest. Now, the cost of living crisis could widen the gulf in fortunes between the city's highest and lowest earners. The capital's public health chief fears those struggling for money could soon face a struggle with their health, too.
Prof Kevin Fenton has worked in many roles focused on public health strategies and has a specialism in tacking disparities.
"More Londoners are moving into poverty, more Londoners are struggling and the economic challenges will have an impact on their health," the senior public health expert, external said.
He explained he believed many Londoners had "fallen backwards" in protecting their health and the lowest earners were the worst affected.
"Wealth enables us to participate in more health-providing behaviours," he said, reflecting on the findings of a recent report., external
He went on to point out that many would have to eat cheaper, less healthy foods and give up costly fitness activities. Furthermore, he worries the stress of financial problems may drive some people to smoking or excessive drinking.
"All of these things can have a huge impact on your health and wellbeing," he said. "But at its core, it's about people having to make tougher choices and people being pushed into more stress, which results in poor mental health, but also less physical health, at this time."
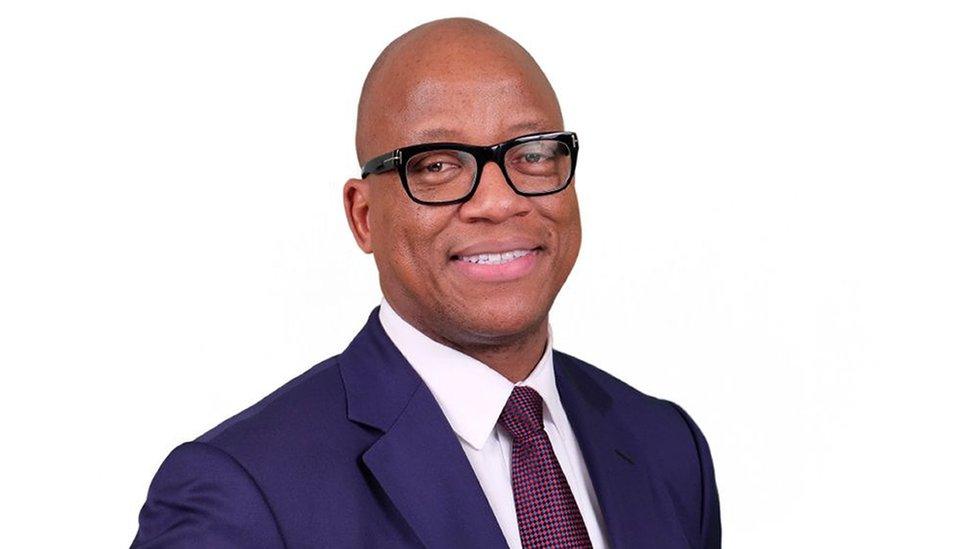
Prof Kevin Fenton, director of public health for London, wants to tackle health disparities
London is historically a city with vastly mixed fortunes.
According to Greater London Authority data,, external wealth inequalities are greater in the capital than anywhere else in the UK, particularly after the high cost of housing is considered.
Prof Fenton's data shows the gap between health outcomes between the most deprived and least deprived boroughs is widening.
On average, Prof Fenton said, a man living in affluent Richmond upon Thames in south-west London will not develop his first major health problem until age 70, but for a man living in the far poorer borough of Barking and Dagenham, the age is 58.
His research also shows that in the most-deprived areas of London, rates of uptake of breast and bowel cancer screening are the lowest, but obesity rates are highest.
But, he said, there is hope. Knowing who needs help and where they are means those people can be targeted.
"We may need to think about where we place services and how we really go deeper into local communities," he said.

The 13,000 residents of the Alton Estate in Roehampton are being encouraged to engage with health service providers
In one such community in south-west London, volunteers do outreach work to connect residents of a large council estate with local health services.
Funded by the NHS and the local council, campaigner Lynne Capocciama runs health-check events on the Alton Estate in Roehampton - home to 13,000 people. She and her team of "health champions" support people to be seen by health services.
She said she started the project because of the "suffering" she saw in her area during the pandemic: "A lot of mental health issues and a lot of people not being able to see their doctor."
One man the BBC met at the centre recently was Derek, aged 63. Thanks to this service, he said, he is aware he is at risk of becoming diabetic.
"I need to, perhaps, cut down on sugar, perhaps a bit more exercise will help me," he said, after learning of his test results.
Ms Capocciama believes many people who come to her events are unlikely to visit their doctor.
"Where I am a resident in the community - people trust me - that's why they're coming to my events and that's why we are having such a good turnout," she said.
The local MP, Labour's Fleur Anderson, said she was concerned about health inequalities in her constituency.
"There's actually a life expectancy difference between living up by the river and living in Roehampton by several years and it shouldn't be like this."

Lynne Capocciama and her "health champions" test people's health in Roehampton
Another big factor in health inequalities, Prof Fenton says, is ethnicity. Diabetes, for example, is more prevalent within black and Asian ethnic groups.
Prof Mark Ashworth, a clinical researcher, analysed patient data from GP practices in Lambeth during a four-year project.
In a paper for King's College London, he said he had found that 47.1% of the black-Caribbean community who visit the GP have long term ill-health. For women of black-Caribbean heritage the figure was 54%, compared with 31% of white British patients.
He said his work also revealed that almost one third of people from deprived areas had long term ill-health comparedwith 19% from less deprived areas.
Prof Fenton said research on this topic could help those who need it most: "Understanding how we see these variations across ethnic groups can have huge impacts on how we provide services, but also how we understand the long-term impacts of those conditions on NHS pressures and the services we need to provide."

Follow BBC London on Facebook, external, Twitter , externaland Instagram, external. Send your story ideas to hellobbclondon@bbc.co.uk, external
- Published14 February 2022

- Published6 July 2022

- Published12 October 2022
- Published22 March 2021

- Published2 May 2020

- Published15 December 2020
