Martha's rule: Son could have been saved with second opinion, father says
- Published
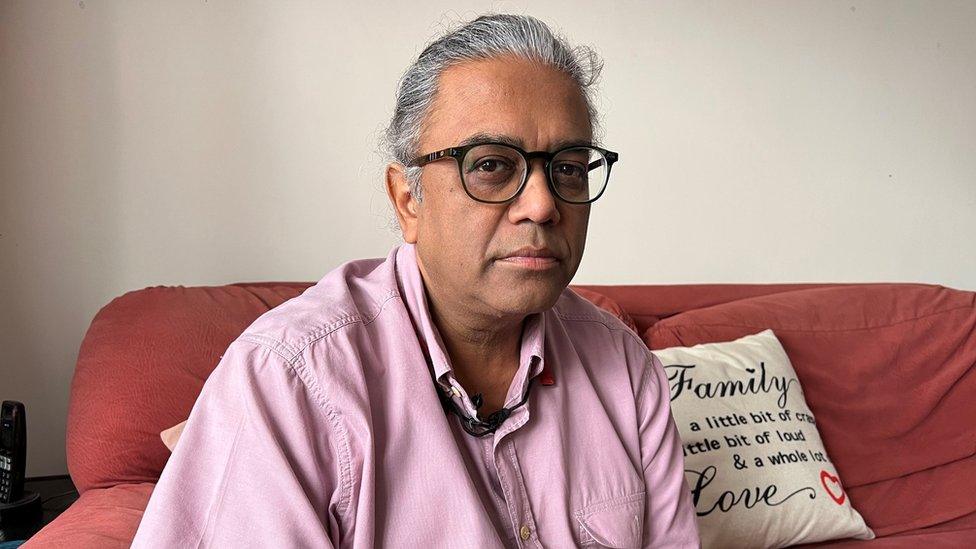
Jay Patel says his son was given treatment that had previously been ineffective
A man would still be alive if his parents had been able to get a second opinion from another doctor, they say.
Balram Patel, 30, from Finchley in north London, was given "unsuitable" treatment that had previously failed to work, his father Jay Patel said.
His lungs became fatally flooded and this cause of death was not initially stated on his death certificate.
It was only after his father intervened, contacting the coroner's office, that it was amended.
The coroner's office has told Mr Patel it is investigating his son's care.

Balram was described as always happy
Guy's and St Thomas' NHS Foundation Trust said it planned to investigate Mr Patel's claims but that it was currently limited as to what it could say until the coroner's investigation was complete.
Balram had multiple disabilities and was developmentally delayed. He was born with half a functioning heart and had liver cancer at the time of death.
He was admitted to St Thomas' in July with a raised infection rate and then suffered a build-up of fluids. It was later decided he should be transferred home due to his vulnerabilities after a Covid outbreak at the hospital.
Doctors discharged Balram with oral diuretics, shown previously not to be effective for him. Mr Patel opposed the decision, explaining his son's medical history, and asked for a second opinion, which he was denied.
At home, the oral diuretics failed to work and Balram began to experience swelling to his feet, calves and hands. His GP sent a letter to St Thomas' urging them to reconsider his treatment.
It read: "This is a failed discharge. They have not put systems in place for this to be supported in the community. We have to now know the orals are not working. You [Mr and Mrs Patel] taking him back is a failed discharge. The discharge was not robust enough."
Mr Patel also said there were not enough district nurses to administer the intravenous diuretics that would have worked in preventing fluid building up in his body.
The family found a surgeon, who was a family friend, who could use an alternative method to give Balram his diuretics through his tissues rather than straight into the bloodstream. But the hospital did not follow up with the surgeon or arrange for him to administer the drugs.
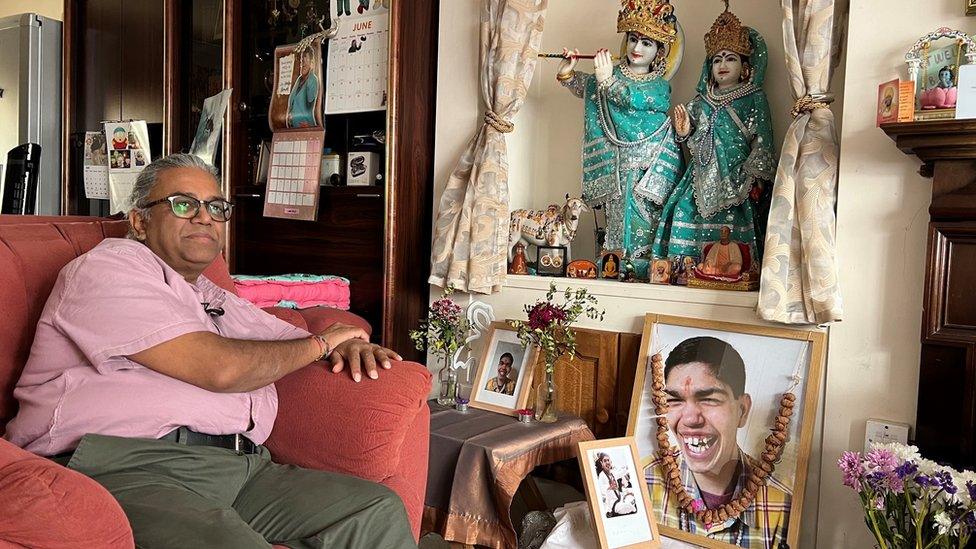
The family say they are devastated at the premature death of their son, Balram
On 8 August, Mr Patel took his son back to hospital on the advice of a palliative nurse. Balram was then administered a dose of intravenous diuretics.
He died in the early hours of the next day from from pulmonary oedema (a build-up of fluid in the lungs). Despite this, the hospital put cardiac failure on his death certificate, with Mr Patel having to fight to have this changed.
He said: "The NHS has been there for us for all of my son's life; Balram was here for 30 years because of the NHS. But because of the same NHS he passed away, before his time and in pain.
"We are absolutely devastated at losing our baby but even more mortified at the early loss of Balram and the huge amount of suffering he endured despite doing, we feel, absolutely everything we could."

Balram with his mother Louise and sister Umika
A spokesperson for Guy's and St Thomas' NHS Foundation Trust said: "We wish to extend our deepest sympathies to Balram's family.
"Balram had incredibly complex health needs and had been under our care throughout his life, during which he was cared for by an extensive multidisciplinary team. Any concerns the family have will be fully investigated."
Since the Balram's death, Mr Patel has set up Patients Lives Matter, a group that campaigns for a legal right to a to a second professional opinion, as well as for an NHS independent complaints investigator.
"I don't want anyone else to ever have to go through something so preventable and since I started [Patients Lives Matter] I've had loads of people get in contact with similar stories of incompetence which has resulted in them losing a loved one," Mr Patel said.
Offering a legal right to a second opinion, known as Martha's rule, is something that is being considered by the government, Secretary of State for Health and Social Care Steve Barclay said last month.
It is named after 13-year-old Martha Mills, who died from sepsis in 2021 following a bike accident. Her mother Merope Mills raised the alarm about the possibility of sepsis but was ignored.

Listen to the best of BBC Radio London on Sounds and follow BBC London on Facebook, external, X, external and Instagram, external. Send your story ideas to hello.bbclondon@bbc.co.uk, external
- Published5 September 2023

- Published5 September 2023

- Published4 September 2023
