Coronavirus: The chaplains at the front line of end-of-life care
- Published

Hospice chaplain Vickie Peters has recorded services to be streamed by video for patients
Coronavirus has radically altered the working life of hospitals. But it has not just affected the doctors, nurses and ancillary staff. While the main role of chaplains - helping patients find a sense of peace - remains unchanged, the way they are doing that has changed beyond recognition.
Lying on a table within the chapel of the Norfolk and Norwich University Hospital is a special document.
On its pages are prayers and blessings for dying patients to be read out not by a person of the cloth but by a member of staff - such as a nurse or doctor - in the event a chaplain is unavailable.
The document's very existence is testament to the immense impact of Covid-19 on the inner workings of the health service.
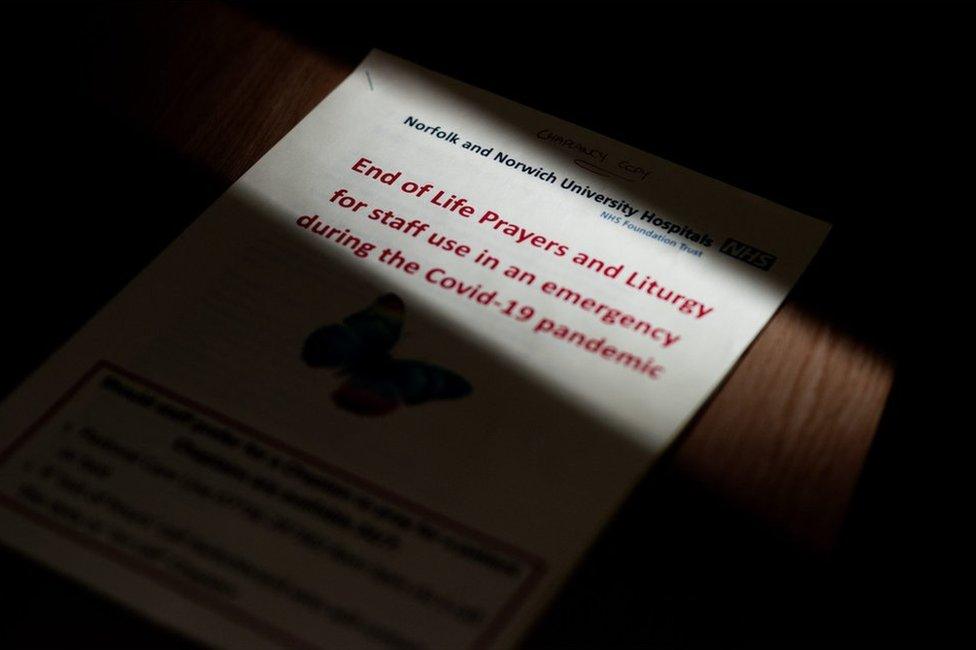
Prayers and blessings for different faiths have been printed out and laminated for nurses to read from if a chaplain is unavailable
Versions of these prayers and blessings have been printed out, laminated and given to the various hospital wards for use in an emergency.
Sometimes, chaplains speak to patients via an iPad - particularly to connect a patient with loved ones.
The hospital's lead chaplain Adrian Woodbridge said: "It's not as good as the presence of another human being guiding you through that process, but it's better than having nothing at all.
"It's somewhere in the middle, and doing the best we can with what we've got."

Adrian Woodbridge in prayer
Mr Woodbridge says the number of Covid-19 deaths is difficult to comprehend fully.
"The danger is we see lots of numbers on the telly. We get numb to them, but those numbers represent human life - people loved, and people that have loved people, that are connected, and their families.
"And one thing about the hospital is we kind of see a glimpse of that, we realise that every life is a human life and it's going to be really missed, and was really loved."

Mr Woodbridge's previous congregation paid for him to have a tattoo on his arm to cover an earlier inking of a scantily clad woman
Sidra Naeem, chaplain at St Luke's Hospice in Basildon, said her role was now confined to telephone conversations.
"It is very, very difficult because 80 to 90% of communication is actually through visual communication.
"You cannot see the patient's expression on their faces, you do not always pick up on their tone of voice or their body language and sometimes a patient could be crying and you do not know.
"And you cannot give them a hug or hold their hand, which is often needed, especially with end-of-life patients."

Sidra Naeem said the coronavirus had wrought havoc on Islamic funeral procedures
Funerals for Muslim patients have been especially difficult, said Mrs Naeem.
"There have been numerous deaths, with a disproportionate number in the black and minority ethnic community, so there has been a huge backlog of burial procedures within the Muslim cemeteries. There have been waiting lists.
"The main thing has been that a lot of Muslims who have died from the coronavirus were not allowed to be washed before burial, which is an Islamic requirement. It is obligatory, really, and they were just buried as they were - covered and then buried.
"And Muslim funerals are usually quite large; usually you can expect 100 or more people to come to send blessings to the dead. But there has been a maximum of six only close family members allowed, which meant that all the other people did not see the burial, which means the grieving process is actually delayed."
For all the pain and anguish that the pandemic has wrought, Mrs Naeem has sought the positives.
"I think everybody has now realised so much of what they had before and now appreciate it. We have a stronger bonding with our families, we appreciate our friends more because we have not seen them, and we appreciate the NHS more.
"It has made us go right down to basics and we are a lot more humble now and we are all one nation, really, facing the same calamity."

Muslim coronavirus patients who have died have not been washed before burial, says Mrs Naeem
Vickie Peters, the lead chaplain at St Helena Hospice in Colchester, Essex, said one of the biggest challenges of chaplaincy amid the pandemic was the distancing, both physical and emotional.
"I think for anyone that is receiving palliative care, obviously their life is limited, and you've got all the anxieties, and physical symptoms that you're dealing with, which is in itself a difficult thing," said Mrs Peters.

The Rev Vickie Peters says she misses the contact she would usually have with end-of-life patients
"It feels like we're not able to show compassion in all the ways that we used to be able to do.
"To me, chaplaincy is about being present with people, it's about being able to hold their hand and look in their eye and to just be with them in what they're going through.
"To have to do that over a telephone, or even through a face mask - it's just not the same connection with people.
"We're now having to record services and put them on YouTube channels for our patients.
"I think one of the challenges for our patients and the families is just a sense of isolation that they are having to deal with."

An inscribed pebble in St Helena Hospice chapel
Before coronavirus, most hospices allowed family and friends to visit freely. That has changed, with visitors often not allowed on the ward unless the patient is at the end of their life - and even then this is subject to severe restrictions.
"I know some of my patients live alone and aren't having carers coming in - they have said to me things like they haven't actually had a face-to-face conversation with another human being since the lockdown started," said Mrs Peters.
"It's just really bizarre, it's like the whole world has changed, the whole way that we're working.
"My role here is to help people find peace in the journey and before they die.
"And I think that's probably more relevant now than ever, really - just helping people deal with anything they've got going on that is getting in the way of them finding peace."
Photography by Laurence Cawley
- Published1 April 2020
