Inside a GP surgery: 'There is not enough time or space in the day'
- Published

The Harborough Field Surgery near Rushden, Northamptonshire, has nearly 13,000 patients on its roll
Not only has the Covid pandemic put GP surgeries across England under immense pressure, it has also caused significant backlogs of work they are now trying to clear. The BBC has spent the morning inside one NHS practice to hear how staff and patients are coping.
The Harborough Field Surgery near Rushden, Northamptonshire, has nearly 13,000 patients on its roll.
Those behind the reception desk say the surgery is almost unrecognisable from how things operated before the pandemic - with telephone appointments, volunteers marshalling the car park and blood pressure readings being sent electronically by patients.
Its nine-strong team of GPs, along with the rest of the staff, are trying to clear the backlog of work which has built up since March 2020.

'There is not enough time or space in the day'

Dr Seamus Kelly says while the pandemic has been "horrendous" it has also forced much-needed change in the NHS
Dr Seamus Kelly, a GP partner at the practice, says the past 18 months have been unlike anything he has previously experienced in the NHS.
"It has been a huge, huge change in everything we've done and all the alterations we've done," he says.
Such changes include how staff deal with patients and each other.
"The whole pandemic has been horrendous," he says. "But there has been some good in there as well.
"The big thing that we've found to be good is the spirit of the staff - they came together and put the extra time in to do the best for the patients.
"The amount of help we've had from volunteers as well, the spirit within the community and within the practice has been great."

Dr Kelly says it is still "impossible" to meet the demand for health care
"The other positive is that developments came along that we'd been asking for for ages and were told couldn't be done - especially technological advancements - have been done," the GP adds.
"People were able to send in their own blood pressure readings electronically, we can do sick notes electronically which had not been able to do, sending prescriptions electronically.
"There has been such a big backlog of work that couldn't be done during the pandemic.
"We've now got to catch up on all of this and there is such huge demand out there that is impossible to meet.
"There is such a huge pressure that there is not enough time or space in the day, no matter how many hours you give to it.
"It is very difficult for the patients who are suffering through this but also for the staff who, after putting in 18 months of hard work, are finding there are not enough appointments and having to explain to patients they cannot get them in today - it is very difficult for them."

'I can usually speak with someone that day'

Linzi Pearsall, 33, lives in Rushden, and was diagnosed with rheumatoid arthritis earlier this year
Linzi Pearsall, 33, lives in Rushden, and was diagnosed with rheumatoid arthritis earlier this year.
She has seen first-hand the immense pressure the surgery has been under.
"It was then that I used to come into the surgery and see how busy they were, especially with the Covid vaccine.
"I actually volunteer now to help out because I saw what a good service they were offering. I thought maybe if I give my time back, I can give back to the doctors at the same time."
You might also be interested in:
"Since my diagnosis I can get an appointment pretty much any time," says Ms Pearsall.
"Obviously I do have to be on the phone at 08:00 [when the surgery opens] but as long as I'm on the phone at that time I can usually speak with someone that day.
"I don't need as many appointments now so if I need any more medicine I'll call up and they will repeat the prescription.
"Sometimes you want a face-to-face appointment which you don't always get. If they think they need to see me, they will call me in.
"As soon as I started having issues I was seen within a couple of weeks - both by the hospital and my GP.
"It has been really hard for people on the front line I imagine, but I think they have done the best they can in the circumstances."

'The treatment for children has been wonderful'
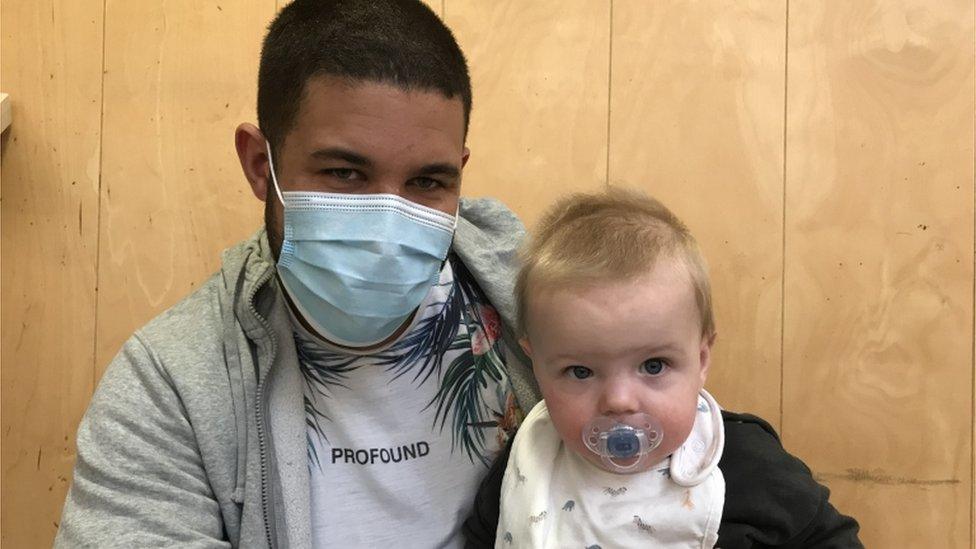
Dwayne tells us his baby boy was recently discharged from hospital after he was diagnosed with Covid
Dwayne, who asked for his surname and son's name to be withheld, was at the surgery because his baby boy, who is less than a year old, had Covid last month.
"We thought it was a chest infection at first and then he was rushed into hospital," he says.
"The treatment for children has been wonderful - for adults, not so good.
"But then again there are a lot more adults out there than children in the world.
"Children, like the elderly, are more vulnerable, so I understand it."

'I don't see it ever getting back to normal'

Hector and Ishbel Graham say some of the changes at the surgery are difficult for older people to adapt to
Hector Graham lives in Rushden and has been a patient at the surgery for about 20 years.
"The whole system has changed," he says. "We can't get appointments to come up and see a doctor. There is a very good triage system run by the practice and they do channel patients correctly.
"I think they've coped very well considering the difficulties they've been under.
"I miss the old style where you could see your doctor and he saw you as a whole person rather than at the end of a telephone.
"They say doctors are happy with the telephone system; a lot of patients are not.
"I was in the health service for 20 years and you looked at a whole person coming in and not a set of symptoms coming in. A lot is lost when you don't see the whole person.
"I would like to see a doctor periodically in person.
"I don't see it ever getting back to normal because there are not enough doctors in the country and we've got an aging population.
"I can see face-to-face consultations being done over the computer and telephone conversations being increased.
"I think the days of 50 people waiting in this room to see four or five doctors are a thing of the past."
Mr Graham's wife Ishbel, who worked in computing during the field's infancy, says: "There's an awful lot from my age group who have never touched a computer.
"Being an older person coming up through the old fashioned ways, well, I think the younger ones like telephone consultations, but when you're our age it is nice to see the face, and to know the face.
"I think the surgeries have been told to adapt and have had to adapt, but I think we could have done with a bit more information for people, especially if they are on their own."

'It's changed completely'

Sophie Lumbis has been business practice manage here for four years
"It's changed completely," says Sophie Lumbis, who has been business practice manager at the surgery for four years.
"We've completely changed the way we work.
"It has been hard, very hard. Everybody is tired, everybody is burnt out - the main thing is trying to keep morale up.
"For me the most difficult thing is trying to keep everybody enthusiastic. Everybody has been incredible."

'We've managed to help a little bit along the way'

Pete McCrone volunteers at the surgery through his involvement with the Rushden & Diamonds
Pete McCrone, lives in nearby Wellingborough, but is working at the practice as a volunteer.
The opportunity came through his football club, AFC Rushden & Diamonds, which set up a group of people who were keen to help in any way they could.
For Mr McCrone, that has meant volunteering to marshal car parks.
"It has been a great deal of fun though it has had its challenges with the weather and people breaking down and that sort of thing.
"We've managed to help a little bit along the way. Car parking can get a bit chaotic when everybody wants to park in the same place."

'The care that I've had has been absolutely brilliant'

Lee Branson (right) is classed as "extremely clinically vulnerable"
Lee Branson is classed as "extremely clinically vulnerable" and has recently been coming each day to see the nurse.
He has his own designated chair in the surgery and has his appointments arranged at quieter times of the day.
"At first the girls had to come on home visits," he says. "When I was on chemotherapy, they brought me my prescriptions and everything.
"I've been here when people have come up to reception and kicked off. But their hands are tied and they can only do so much.
"The care that I've had has been absolutely brilliant."

Find BBC News: East of England on Facebook, external, Instagram, external and Twitter, external. If you have a story suggestion email eastofenglandnews@bbc.co.uk, external
- Published9 September 2021

- Published13 May 2021

- Published8 March 2021

- Published23 February 2021

- Published23 December 2020

- Published17 December 2020
