Nottingham maternity crisis: What are families calling for?
- Published

As a review gets under way into maternity services in Nottingham, the BBC looks at how the city's hospitals came under the spotlight, and speaks to parents about what they hope the investigation will achieve.
What happened at the hospitals?

Wynter Andrews died 23 minutes after being born on 15 September 2019
In October 2020, two cases came before Nottingham Coroner's Court.
Both of them involved babies who had died shortly after being born at the city's hospitals.

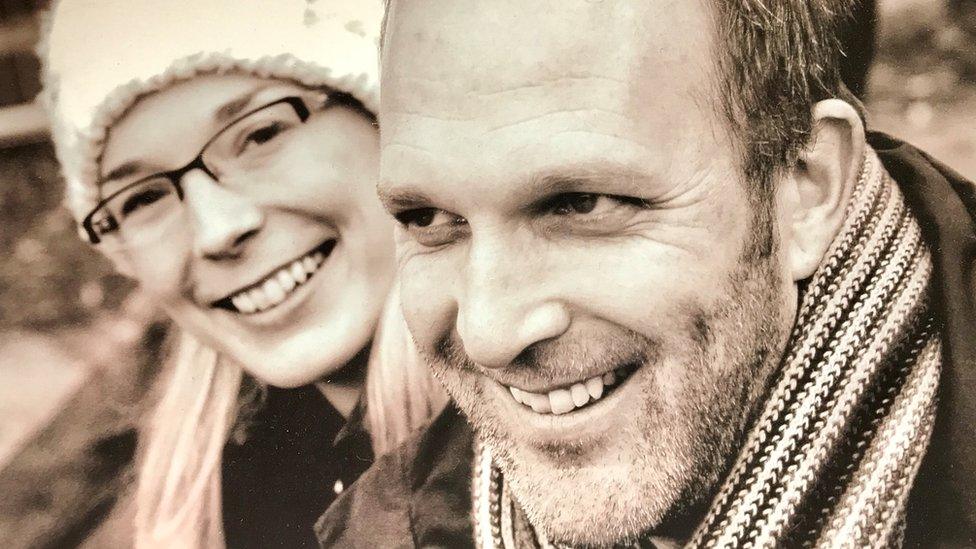
Sarah and Gary Andrews now have a nine-month-old son
Wynter Andrews was delivered by Caesarean section on 15 September 2019 at Nottingham's Queen's Medical Centre (QMC) and died 23 minutes later.
The court heard concerns over the conditions of the baby and mother were not acted on.

The coroner said Wynter's death was a "clear and obvious" case of neglect
Assistant coroner Laurinda Bower said it was "a clear and obvious case of neglect".
In the case of Kouper Needham, who died of respiratory complications in July 2019 after being discharged, Miss Bower ruled his discharge had been appropriate.
However, she did criticise the trust's feeding policy at the time and noted the family were dissatisfied with Kouper's care.

In the case of Kouper Needham, the coroner noted the family were unhappy with his care
These families - and others who were unhappy with Nottingham's maternity units - came together to call for change at the Nottingham University Hospitals (NUH) trust, which was set up in 2006 to run the City Hospital and the QMC.
Among their number were Jack and Sarah Hawkins, who received a £2.8m settlement in 2021 over the care of their daughter Harriet who was stillborn at the City Hospital in April 2016.
It is believed to be the largest payout for a stillbirth clinical negligence case.

Sarah Hawkins' daughter was stillborn in 2016
Mr and Mrs Hawkins - who had themselves worked for the trust in the past - said that in the days leading up to the stillbirth, they were repeatedly told by NUH that Mrs Hawkins was not in labour.
"I was made to feel like a complete failure, like I was the only woman who couldn't deal with labour," she said.
"I just remember lying on the sofa, saying 'no-one's helping me'."

Jack Hawkins pushed for an inquiry into the maternity services at Nottingham University Hospitals
Eventually Mrs Hawkins was admitted to City Hospital and, as she was preparing to give birth, a midwife tried to check Harriet's heartbeat but failed to find it.
"Two senior midwives came and they couldn't. Then the doctor came and said he couldn't find it because my bladder was full," she said.
"The doctor drained my bladder. Then he scanned and said 'I'm sorry, your baby's dead'.
"I just went numb from head to toe. It felt like an out-of-body experience.
"I thought 'This isn't real. This is a nightmare'. I was a low-risk, healthy pregnancy. Everyone was telling me I wasn't in labour.
"I was then left for nine hours trying to deliver her on my own because the consultant wasn't aware that I hadn't delivered her. I felt like I was dying. I was so exhausted."
The couple say they never felt believed during or after labour
The couple have pushed for an independent, external review since the loss and said the trust has been "desperate" for the truth not to come out.
"I was never believed in labour; I was never believed after labour. It was absolutely horrific for that to happen and we don't believe that's ever been acknowledged," Mrs Hawkins said.
"It's been completely swept under the carpet. Three years after Harriet died, Wynter Andrews died and the coroner found neglect. It was basically nearly a copy-and-paste of my labour. We have met so many families with dead babies and harmed mothers.
"It's evidenced by harmed people. I don't know how people can't - to this day - understand that or address it."
Have other concerns been raised?

Sue Brydon said there didn't seem to be "any workforce planning"
Alongside the families, other voices also expressed concern about the trust's maternity services.
In 2018 Sue Brydon - a senior midwife at the QMC - wrote a cry for help letter.
Ms Brydon, who has now retired, said her concerns focused on low staffing levels alongside increased demands on the labour suite, with the number of complex, high-risk births increasing.
"I wrote that letter but... it was signed by a majority of the staff that were able to sign it," she told the BBC.
"It was absolutely raging because I had in my own experience spent some time as acting head of midwifery and one of the things that I knew how to do very well was workforce planning.
"In Nottingham we always had a good number of people who wanted to train as a midwife and if you train midwives you can fill your posts.
"That just seemed to fall apart and there didn't seem to be any workforce planning and the numbers of vacancies were quite large but we were told that there weren't any vacancies.
"The stress at the bottom was enormous. When we presented the letter to the trust board, we had no real idea just how bad it was.
"We did know the service... was teetering on the brink."
Up until 2020 maternity services were rated good by hospital inspectors.
But in an inspection published in December of that year, they were rated inadequate with the Care Quality Commission (CQC) finding "several serious concerns", including staffing, poor leadership and a culture that did not learn lessons.
Two years on, services remain inadequate and the CQC are seeking to prosecute the trust over the death of Wynter Andrews.
In 2021, an investigation by Channel 4 News and the Independent reported that 46 babies suffered brain damage and 19 were stillborn in Nottingham between 2010 and 2020.
More than £91m in damages and costs were paid out, according to the report.
A Freedom of Information request by the BBC found more than 160,000 babies were born at the units between 2005 and 2022.
In that time, there were 207 claims resulting in pay-outs, with most claims for failure or delay to treatment and a failure to respond to abnormal foetal heart rate.
What are families calling for?

Donna Ockenden was brought in to lead the review of Nottingham's maternity services
Families joined forces and spent years campaigning for an independent review into the trust's maternity units.
A review had been set up by the local clinical commissioning group (CCG), NHS England and NHS Improvement but it came in for considerable criticism, with families questioning its independence and the experience of the team behind it.
In April, dozens of families wrote to the government expressing concern about the review and calling for Donna Ockenden, who led the inquiry into the UK's biggest maternity scandal at Shrewsbury and Telford NHS Trust, to take charge.

Ms Ockenden investigated almost 1,600 incidents at Shrewsbury and Telford Hospital NHS Trust
In May, it was announced Ms Ockenden would lead a new review.
She has said she was "absolutely honoured" to be chosen for the role.
Her review will get under way on Thursday.
It is set to last about 18 months - depending on the number of families who come forward.
How do families feel now?

Michelle Welsh felt "traumatised" by her treatment when she gave birth to her son Billy
Families have cautiously welcomed the review but have said it is essential the results are listened to.
Michelle Welsh, who is a Labour councillor for Nottinghamshire, and sits on the health scrutiny committee, said she felt "traumatised" by her treatment when she gave birth to her son Billy.
She said: "My worry is that NUH thinks Donna Ockenden is coming and everyone stands back.
"We still need to see evidence of improvements and NUH. I am concerned NUH think it's resolved and it's not resolved.
"That's why it's really important the government needs to be there to back Donna Ockenden up.
"We cannot allow families, who have been through the most traumatic experiences imaginable, to keep standing up and fighting. It has done untold damage to people.
"It is a very long time for women to be receiving poor care, for women and children to be dying needlessly and for families to be suffering unnecessarily.
"How has it been allowed to go on and why has it taken parents to bring this about? It enrages me that women and babies have been put at the centre of this.
"Somebody at NUH needs to answer that."

Michelle said William - known as Billy - is her "absolute world" - but says her story could have been so different
A Department of Health and Social Care spokesperson said: "It's absolutely vital that mothers and babies have access to the best possible care.
"Donna Ockenden has brought a wealth of experience, particularly following her work on the review of Shrewsbury and Telford maternity services - and the department looks forward to seeing her recommendations for urgent improvements.
"We will continue to take all the steps necessary to ensure no families have to go through this pain again."
What does the trust say?

Sharon Wallis says improvements will take time
Sharon Wallis, head of midwifery, said it was important lessons were learned.
"We've made lots of improvements: making sure our systems are joined up, we've implemented a maternity advice line which is staffed 24 hours a day.
"We are doing lots of work around recruitment and the culture around the organisation but this is not going to be an overnight fix.
"This is going to take some time and that's the frustrating thing for everybody."
She said the trust needed to fill around 65 vacancies which was a similar picture across the country.
Privately, Ms Wallis has expressed concern that the media are painting "a damning picture" of the service.
A leaked memo to staff revealed she felt the trust's "great work" was being left out of coverage of the service.
Hospital bosses "wholeheartedly apologised" for offence caused.
How does the picture compare with other trusts?
Comparison data between different hospital trusts is not straightforward, due to the differing size and demographics.
Ms Ockenden herself has said Nottingham is a "very different" maternity service to Shrewsbury and Telford, the subject of her previous report.
"It has two big units at Queen's Medical Centre and at the City campus," she said.
"What is really important is that we come to Nottingham with fresh eyes.
"I think that what we can bring is a real commitment to family voices being at the heart of everything we do."

Follow BBC East Midlands on Facebook, external, Twitter, external, or Instagram, external. Send your story ideas to eastmidsnews@bbc.co.uk, external.
Related topics
- Published10 July 2022
