Pioneering Middlesbrough heroin addiction clinic to close
- Published

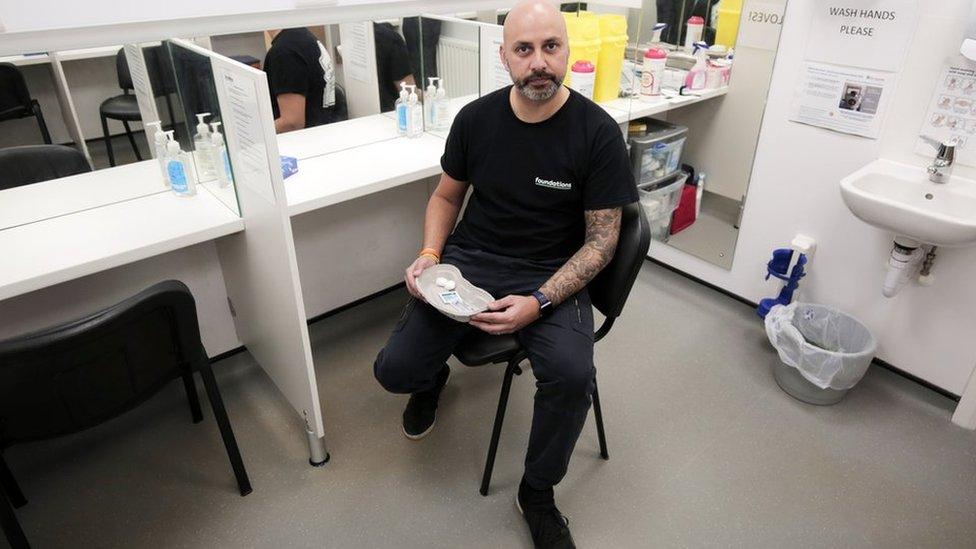
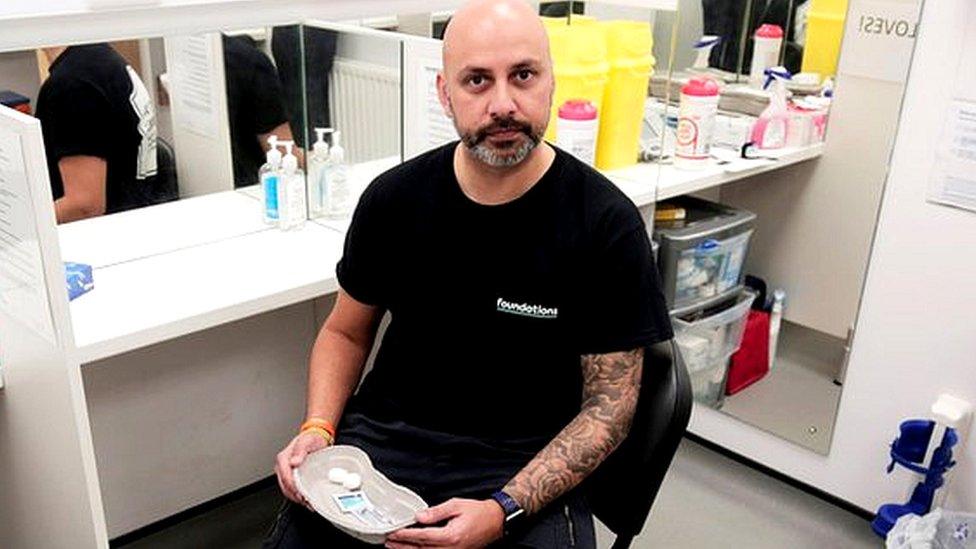
Danny Ahmed set up the Middlesbrough clinic in October 2019
A ground-breaking clinic for people tackling heroin addiction is set to close because funding has run out.
The Heroin Assisted Treatment (HAT) programme in Middlesbrough was the first of its kind in England when it opened three years ago.
It is offered to patients who have exhausted all other options and allows them to self-administer diamorphine twice daily under medical supervision.
Clinicians have described the decision to end funding as "ludicrous".
The north-east of England has the highest rate of drug-related deaths in the country, according to figures released by the Office for National Statistics last month, external.
Since 2017 it has risen by 39% and, although a much smaller number of individuals, Middlesbrough's death rate is up 80%.
'Devastated for patients'
At HAT, heroin dependency is viewed as an illness.
The goal is eradicate each patient's need to commit crime to buy street heroin. Instead, they can focus on their health and engage with wrap-around support.
It is an approach that is used in other countries, such as Canada and Germany.
It costs £12,000 to put a patient through treatment for a year and is usually reserved for those who have not benefited from any other type of treatment.
Danny Ahmed believes the scheme has been a proven success
Clinical lead Danny Ahmed described the programme's closure as "a tragedy for everybody involved... the patients, the staff but also the wider community".
He said: "What we've shown over the last three years is that we've been able to reduce crime locally.
"We've been able to improve the health and the wellbeing of the participants and that has had a significant impact on community cohesion.
"I'm devastated for the patients that are currently on the programme and I'm frustrated.
"Healthcare is all about evidence-based interventions, we've added to the evidence base that this is a successful treatment option. It's been shown to be successful across the world and it's been successful here in Middlesbrough.
"It's ludicrous that we're in a position where it's no longer being funded."

James's story

James Fowler was born into a home of alcoholics and drugs were an ever-present in his childhood.
He got hooked in his early 20s and, before long, was using heroin and crack cocaine.
Shoplifting and spells in prison followed, all the while his drug use escalated.
Then he was introduced to HAT.
Now the 41-year-old is studying humanities and social science at Middlesbrough College with an ambition to get a degree in psychology.
"It's really hard at college but I wouldn't swap it for the world," he says.
"On the streets you're just begging for money or shoplifting but every time you do that you're throwing a little bit of your life away. You're constantly living in that world of pain. I'm so much more at peace with where I am now.
"It overwhelms me and I feel like I have imposter syndrome. Life used to be very different."
Escaping his old life is "difficult", dealers still recognise him on the streets, but he's focused on "bettering himself" and works part time as a chef in town.
"I'm trying to act like the real me but it feels alien. I see people who've gone on treatment and they're doing well. I'm attracted to what they have. It feels right. I'm being directed by my heart and not my head for once."
Before receiving diamorphine treatment, James had burgled the house of his mum's partner for money to buy crack.
"Although I was there and very present and remember doing it, it feels like we're talking about somebody different.
"My mam's just started coming back in to my life. I haven't made amends properly yet but she's really proud.
"She rings me all the time. I can see her fears edging away."
James remembers his first time in the HAT clinic as "weird" but he felt safe.
"I didn't feel like I had to hide away in the shadows to use or put myself in dangerous situations to go score."
He disappointed to hear the clinic is closing and hopes the current patients can find an "alternative pathway to recovery" that works for them.

When HAT began in 2019 it was criticised for using public money to give people free drugs.
Seed-funding was provided from the budget of former Cleveland Police and Crime Commissioner (PCC) Barry Coppinger.
The Labour commissioner estimated the crimes of the first 15 patients cost the force about £800,000 over a two-year period.
His successor, Conservative PCC Steve Turner, decided not to renew funding from his budget when he was elected last year.
Stopgap funds were found by South Tees Public Health and Operation Adder, external - but both parties are no longer able to support it.
Mr Turner regards HAT as "very much a public health initiative".
When asked about its demise, he accepted it had been positive for recipients but rejected the impact warranted cash from his budget.
An independent study by Teesside University, external, published last year, found the treatment had economic value, as well as health benefits to participants and a "large reduction in criminal behaviour".
It concluded that in the first six months of treatment, the first six patients committed three "lower-scale offences", whereas previously the same individuals had committed 541 detected crimes, with an estimated cost of £2.1m.
Cleveland's Police and Crime Commissioner Steve Turner axed funds for the scheme last year
However, Mr Turner is not convinced it is evidence of long-lasting reduction in criminal behaviour.
"Where you've got somebody who steals to fund a habit, you're always going to get an anecdotal reduction in crime," he said.
"What doesn't happen is when you take five, six, 10 addicts and stop them stealing…You're not actually doing anything to cut crime as a whole.
"If you take the money and invest it in programmes that affect 100s of people instead of 10s - that's better value of combating the crime element of drugs.
"If a programme isn't cost effective, market forces will close it down.
"I have never said the programme does not work for the individuals on it. The HAT programme has had a fantastic opportunity to prove to others up and down the country, public health authorities, the government and other PCCs that they've got a programme that they believe in.
"Is it the best way to spend money to combat drugs? That's for other people to decide."
Middlesbrough's Labour MP Andy McDonald called the decision to stop funding "short-sighted, counterproductive and frankly wrong".
"The consequences are obvious. We will see an increase in street drug activity, poorer health and more crime and disorder," he added.
Mr Ahmed says he is "hopeful but doubtful" that alternative funding can be found to rescue the service.

Follow BBC North East & Cumbria on Twitter, external, Facebook, external and Instagram, external. Send your story ideas to northeastandcumbria@bbc.co.uk, external.
Related topics
- Published9 December 2021
- Published7 July 2021

- Published24 February 2020