NI health 2019: A year of momentous health stories
- Published

It's been a year of significant and momentous health stories in Northern Ireland and just when you thought it couldn't get any worse - it often did.
Month after month brought difficult and contentious issues, so much so, that by December the health service finally appeared to be near tipping point.
And there's no sign of things abating.
As we step into 2020, many critical matters hang in the balance as reports await unpublished, investigations continue and more strikes loom.
The BBC reported extensively on hospital waiting times, the neurology review, Muckamore Abbey Hospital, abortion and hyponatraemia to name just a few.
The year culminated in strike action by almost 20,000 health and social care workers.

The unprecedented action appeared to sum up the frustration and all out sense of crisis and hopelessness that's enveloped health and social care.
The last official figures for the year revealed more than 300,000 people were waiting to see a consultant - the highest ever across the UK.
Cancer targets also continued to be missed with one in five cancer patients receiving their diagnosis in an Emergency Department.
A special BBC News NI report examined waiting times and prompted the independent think tank, the Nuffield Trust, to warn that parts of Northern Ireland's health care system had already collapsed.
The Royal College of Surgeons followed. GPs, nurses and other health care professionals said they have been predicting the fall for years.

Northern Ireland's health crisis grabbed the attention of national audiences with our waiting list figures splashed across broadsheets and network programmes
Health's permanent secretary Richard Pengelly said it would take £1bn to tackle the problem.
'No time is a good time'
According to the health unions, repeated warnings for better workforce planning and funding were ignored, others argued leadership was lacking while the political vacuum exacerbated it all.
The health unions said industrial action and strike were a last resort.
Their response to achieving pay parity and safe staffing could not have come at a worse time.
But they argue that no time is a good time.
Thousands of appointments and numerous operations were cancelled; some people who'd already been waiting for years will now have to wait even longer.
Despite [pre-election] purdah preventing interviews being allowed on other significant issues, talks around pay prompted several senior health officials to speak out.
Dr Michael McBride told the BBC that compromise from all parties was required and he urged everyone "to step back, pause and resume negotiations".
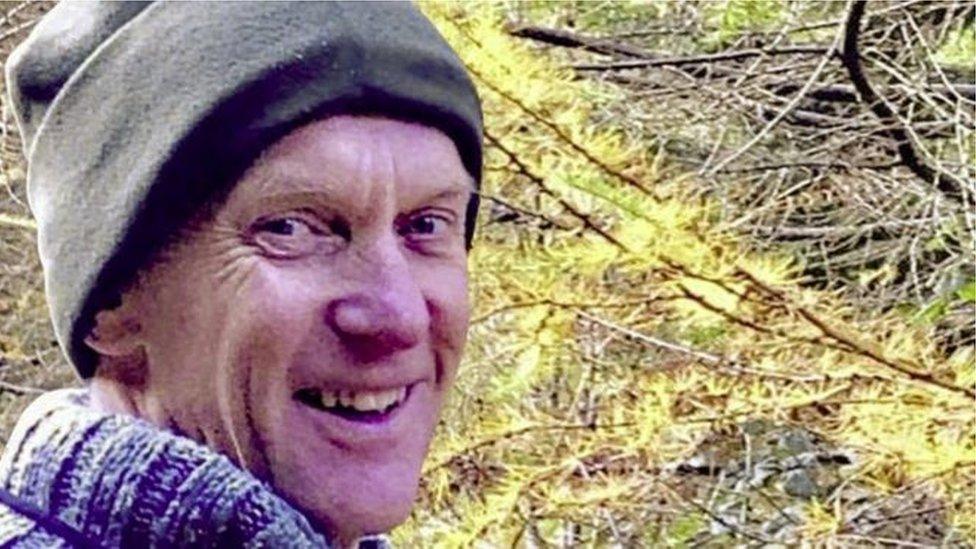
Dr Michael Watt worked at the Royal Victoria Hospital as a neurologist
Muckamore Abbey Hospital
A joint statement from the six health trusts was also issued and the Secretary of State, Julian Smith, managed to reconvene talks but a new pay offer was declined.
The Permanent Health Secretary, Richard Pengelly having just stepped out of talks with the health unions spoke live to BBC Newsline saying he did not have the authority to deliver pay parity which required overturning a policy by a democratically-elected minister.
Muckamore Abbey Hospital and the neurology recall also dominated headlines.
While shocking allegations of abuse and ill treatment of patients at the Antrim Hospital began to surface in 2017, two years later the PSNI is now involved and a major investigation is under way.
In 2017, it was revealed four staff members had been suspended and the BBC reported that the allegations "centred on the care of at least two patients".
Parents have broken their silence and, in heartbreaking interviews, details have emerged of their children's ordeal.
Thousands of hours of CCTV footage have been viewed, more than 40 staff members have been suspended and several arrests made.
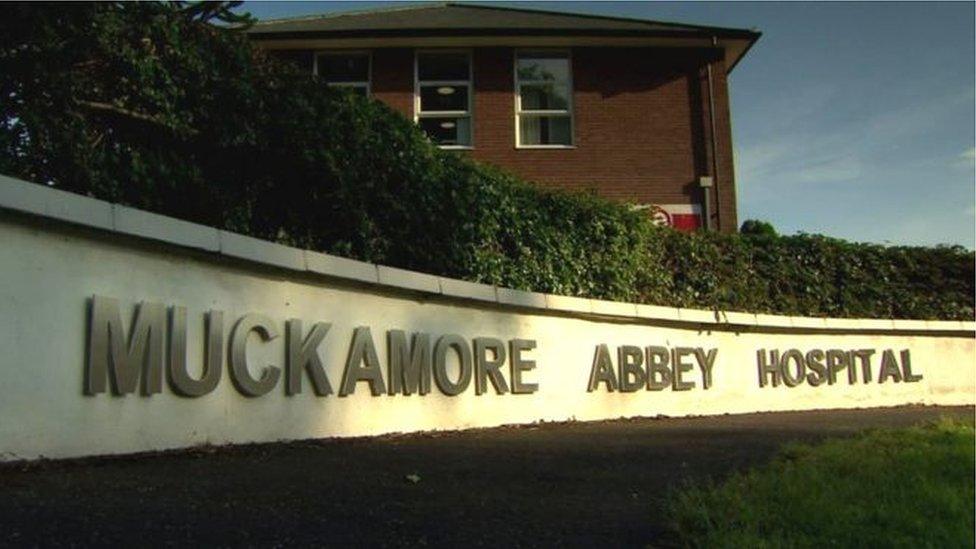
In an exclusive interview with the BBC, the chair of the biggest review into NI's mental health services, Roy McClelland, said the crisis at Muckamore Abbey Hospital "could be the tip of the iceberg".
'Disturbing'
He described testimonies from parents of adult children with profound learning difficulties as a "disturbing listen".
Richard Pengelly's commitment that no one would call Muckamore their home by the end of the year has not been achieved.
The BBC revealed that 39 patients have had their discharge from hospital delayed.
Meanwhile, the long-awaited report into Northern Ireland's largest patient recall was finally published just days before Christmas.
Despite that, there remains much confusion and many unanswered questions for hundreds of neurology patients.
In May 2018, the BBC revealed the detail around the extent of the crisis including that the suspended Belfast neurologist Dr Michael Watt had carried out hundreds of unnecessary procedures on patients - some of whom were possibly misdiagnosed with life-changing conditions including Parkinson's and MS.
'Sincere sympathy'
It took a BBC Spotlight investigation to reveal the impact of what happened - the programme threw light on Dr Watt's practice including the misuse of epidural blood patches.

BBC Spotlight's Conor Spackman spoke to some of Dr Watt's patients
Earlier in the year, it was revealed that an official hearing into the actions of Dr Watt had been delayed until 2020.
While the doctor remains suspended, many patients say their lives are on hold until they find out why he was allowed to practice as he did and who, if anyone, was monitoring his workload.
In a statement to the BBC, Dr Watt offered his "sincere sympathy" to those affected by the recall.
Dr Watt said he recognised the "distress these events have caused".
Dr Watt also previously stated that he had done his best and sought to act in the interests of his patients while handling a big caseload and that this was against the backdrop of a shortage of neurologists and that he felt that he was being scapegoat and used as "a political football due to the upcoming election".
'Children's stories'
He said: "Patient care has always been of the utmost importance to me and the key focus throughout my career.
"I have always sought to act in the best interests of my patients."
Children's stories featured, too.
Remember Aimee Brady? The 11-year-old Magherafelt girl made a public appeal for greater discussion around organ transplants.

Aimee Brady passed away in October
Sadly, Aimee's wish was never granted and she passed away in October while waiting for a heart.
We also heard from 14-year-old Lauren who has a rare form of cancer, neuroblastoma.
She helped launch a story book which explains medical terms to kids. Lauren is taking part in a clinical trial in New York.
And what about Reuben, the boy who reacted when news emerged that Northern Ireland's cystic fibrosis patients were to benefit from the drug, Orkambi.
With arms in the air he said with a smile across his face: "We got the drug."
Abortion was decriminalised.

Despite decades of political and legal deadlock, the dramatic move happened almost seamlessly at Westminster taking everyone by surprise.
The law changed, which means women and girls can terminate a pregnancy without fear of being prosecuted.
That possibility of prosecution is also lifted from healthcare workers.
Northern Ireland is now in an interim period - much still has to be resolved before it ends at the end of March.
While the legal move cannot be overturned, thousands of people are deeply unhappy and vow to continue with their "no change to the law" campaign.
We managed to explore a lot of things this year including many issues around women's health.
Light was shone on the issues of cancer of the vulva, smear fear and endometriosis.
It took brave women to step forward to talk about their most intimate parts - while the rest of us were educated. Hopefully the policy-makers were listening.
As we move into 2020, it looks like Northern Ireland's political parties are on the verge of restoring the political institutions.
At the time of writing, it hasn't happened yet. Whatever the outcome, Northern Ireland's health and social care service needs a huge injection of energy, focus, funding and, perhaps critically, leadership.
As it is a leap year - perhaps we will see some prepared to take a huge step forward.