Northern Ireland's antidepressant spend increases by £7m in 2020
- Published

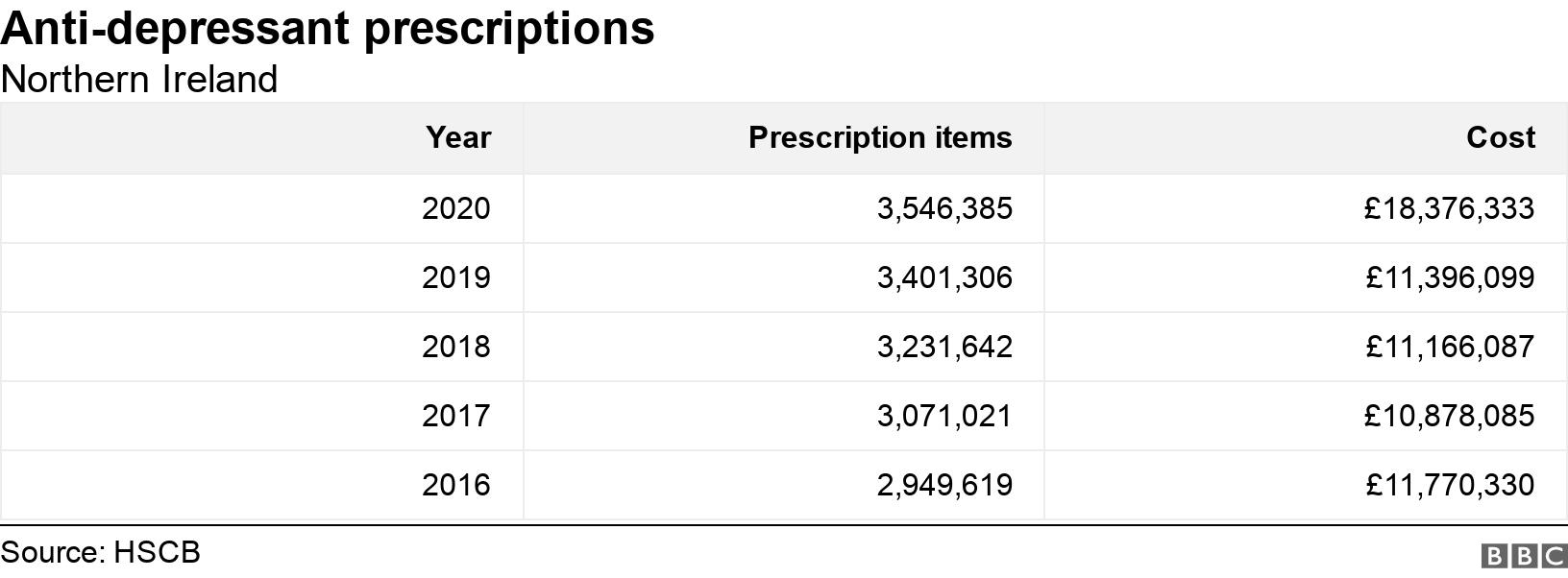
The amount spent on anti-depressant drugs in Northern Ireland has increased by almost £7m in just a year.
Figures show that expenditure went from £11.3m in 2019 to £18.3m in 2020.
Health officials say price increases among some of the most commonly used anti-depressant drugs have led to a "significant impact" on costs.
Responding to the figures, a leading GPs' union raised concerns about the "tsunami of mental health issues" caused by Covid-19.
Anti-depressant drugs can be used to treat a number of conditions such as anxiety and depression, and they are one of the most commonly-prescribed medications in the UK.
Previous research has found that Northern Ireland has one of the world's highest prescription rates for anti-depressants.
'Significant increase'
The Health and Social Care Board (HSCB) publishes an annual list of all drugs prescribed in primary care in Northern Ireland.
in Northern Ireland 2020
3.5mprescriptions items
£7m cost increase between 2019 and 2020
£3.35per item in 2019
£5.80per item in 2020
Community pharmacists dispense the prescription drugs referenced in the HSCB figures. The price that pharmacies are paid for medicines dispensed in Northern Ireland are set by the Department of Health in London.
In recent years the Department of Health has increased the reimbursement price it pays to community pharmacies because of higher prices being charged by suppliers.
For example, Sertraline is one of the most common drugs used to treat symptoms of depression and anxiety in Northern Ireland. HSCB said price increases in such drugs had led to a "significant" increase in costs.
"Price increases among some of the most commonly used anti-depressants such as sertraline, venlafaxine and duloxetine, have led to a significant impact on costs within the anti-depressants group of drugs in 2020," said a HSCB spokesperson.
"For example, the drug cost of sertraline (50mg) increased from £1.27 for a pack of 28 in January 2020 to £6.46 in March 2020."
Gerard Greene, Chief Executive of Community Pharmacy NI said reduced supply and higher prices meant the Department of Health had to "revise the prices it paid to pharmacies and this has contributed, in part, to the increased anti-depressant expenditure that has been reported in Northern Ireland".
'Tsunami of mental health issues'
The Royal College of GPs said the prescription figures highlighted a worrying trend, particularly during a year when the population was in lockdown for a significant part of the year because of Covid-19 restrictions.
The organisation's Northern Ireland Chairman, Dr Laurence Dorman, said: "The Covid-19 pandemic has caused a tsunami of mental health issues which GPs are witnessing and managing in communities across Northern Ireland.
"Unfortunately, prescribing medication is only part of the solution when managing mental health needs."

He added: "Ideally, for depression and other mental health conditions, GPs would have a wide range of treatment options available to them, such as counselling.
"Unfortunately, for too long these services have not been timely or easily accessible."
Last month the Participation and the Practice of Rights (PPR) group highlighted concerns that Northern Ireland operates a "postcode lottery" for people who need access to counselling.
"There is a clear connection between, on the one hand, the exponential rise in prescribing rates for anti-depressants, and on the other, the ongoing failure to adequately resource counselling as an effective treatment option for mental health," said PPR's Sara Boyce.
"As the mental health impacts of the pandemic begin to be seen, GPs now more than ever need to be able to provide timely access to counselling alongside or instead of medication," said Ms Boyce.
She called on Northern Ireland's Health Minister Robin Swann to ensure the strategy included timely, local access to counselling for all who need it.
Drug misuse
Diazepam was involved in a third of Northern Ireland's 191 drug-related deaths in 2019, with pregabalin being a feature in more than 40%.
Diazepam is commonly used to treat anxiety and seizures, while pregabalin is typically used to treat pain, anxiety and epilepsy.
Earlier this month a mother from west Belfast, who lost her son to drug misuse, urged the Stormont Executive to create a service that treats mental health issues alongside drug and alcohol addiction.

Prof Siobhan O'Neill says anti-depressants can be a very useful treatment for depression
While the latest figures are concerning, it was also important to remember anti-depressants had a legitimate use for some people, said Northern Ireland's Mental Health Champion.
Prof Siobhan O'Neill said: "Anti-depressants can be a very useful treatment for depression, however they should be taken under the supervision of a doctor, and should usually be accompanied by the option of non-pharmacological treatments such as counselling or psychological therapy.
"I am concerned that many people in Northern Ireland who express a preference for a talking therapy, do not have the option of having psychological therapy or counselling due to long waiting times, or poor availability of services locally."
Health officials say other possible reasons for the increase in the use of anti-depressants in Northern Ireland may include greater awareness and improved diagnosis of depression and other mental health conditions.
Related topics
- Published16 November 2014

- Published18 March 2021

- Published12 March 2020
