NI Health: 'More people than ever paying for private healthcare'
- Published
- comments
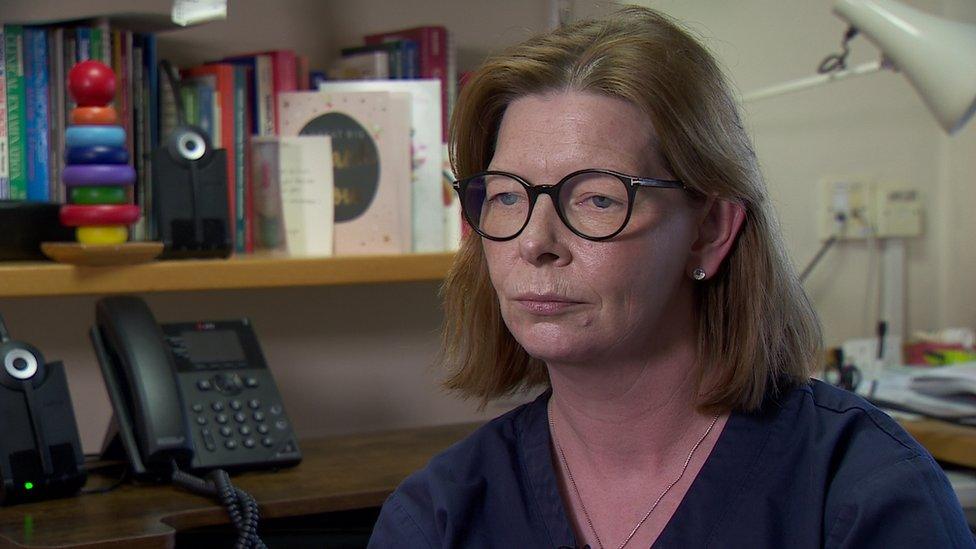
Dr Ursula Mason is chair of the Royal College of GPs
More people than ever are having to use private healthcare which could mean more people getting into debt.
That is according to the chair of the Royal College of GPs in Northern Ireland.
Dr Ursula Mason, a GP in Carryduff, said there had been a "significant rise" in patients having their "health needs met in the private sector".
She added the scope of such treatments had expanded beyond the traditional hip or knee replacement.
"More often than not people are putting their hands in their pockets and asking family, perhaps, to fund private care," she said.
One independent hospital in Northern Ireland, Kingsbridge, has reported a 33% increase in footfall between 2021 and 2022.
The hospital's chief executive, Mark Regan, said there was no longer an "elitist aspect" to those who came to them; instead it was "everyone... because they simply can't wait" and are "seeking other options".

Mark Regan says that there is no longer an "elitist aspect" to people using the private sector
According to research by the Institute for Public Policy Research (IPPR) think tank, a long-term decline in access to health services has been rapidly accelerated by Covid-19.
As a result more people have bought private health insurance or paid for treatment.

'Why I paid for private treatment'
Philip Stevenson paid privately to get cataracts treated in one eye.
The operation cost £3,000 and the 75-year-old is on a waiting list to have his other eye treated.
'I paid £3,000 for my eye operation'
A part-time lorry driver, he said he had no option but to pay privately or "sit and do nothing, vegetate and slow up".
"I was very lucky that I could afford to pay for it, more fortunate than other people, and I felt if I go private I am helping the health service as someone else can have my place."
He said he did not think it was fair he was facing a wait of two or three years: "I didn't like it (going private) but that's the way it is."
Brian McKeown is the vice-chair of Optometry Northern Ireland and has three practices in Northern Ireland.
He treated Mr Stevenson and said his experience was becoming more common.
"Back in 2019 our stats for referring patients privately for cataract surgery was about 10-20% of the patients we see and now that's completely flipped," he said.
"In 2022 it was about 60-70% of patients we chat to who have cataracts and then are thinking - 'can I wait for NHS surgery or do I need to try and find some money and try and go privately?'"

Dr Mason said Northern Ireland was already in a two-tier health system.
"We are seeing more and more patients choosing to go down the route of private healthcare perhaps financially detrimentally to themselves - they are getting into debt which will have a knock-on effect further down the line," she said.
Mark Regan said many people could no longer afford to wait: "Your health is a one off, you have one opportunity and therefore people are finding other ways. They may not be buying new furniture, or changing their car or going on a foreign holiday.
"This is a choice people are making as they can't get access in other routes."

Everything changes and nothing stands still - so said the Greek philosopher Heraclitus.
Fast forward two millennia and his thinking can be applied to many things including the health service.
Seventy five years old this July, the NHS is painfully realising that it too is changing and having to provide an awful lot more than what it set out to do in 1948.
Back then it dealt mostly with infectious diseases and the effects of malnutrition.
Today it is knee and hip replacements, innovative brain and cancer surgery and, thankfully, keeping an increasingly older generation in better health.
The fact is a two tier health system already exists with the poorest losing out.
In fact, people are now having to wait within the private sector too.
Might a three tier system emerge?
In one independent hospital, waiting lists for gynaecological surgery have crept into August.
Consultant surgeon Mark Taylor said, considering the waiting lists, there was room for both sectors.
The challenge, he said, was having the two working in tandem to make healthcare accessible to all.

The Department of Health (DOH) said it wanted a health service that provides timely care to everyone who needs it when they need it.
A spokesperson added: "We are clearly a considerable distance from this goal, the route to get there has been clearly mapped out.
"It will require sustained action to increase hospital capacity through both investment and reconfiguration of services.
"Reconfiguration is underway with the establishment of Day Procedure Units and Overnight Stay Centres."
The DOH also said "significant funds have been used to secure additional capacity from the independent sector".
It said in the first nine months of 2022/23, a total of 91,668 assessments, diagnostic tests and treatments were purchased from the independent sector by the HSC system.
Nigel Edwards is the chief executive of the independent health think tank, the Nuffield Trust.
He described the general trend of people turning to the private sector because they felt they had no alternative as "quite worrying".
"The whole premise of the NHS is that we all pay in and then we all get benefits that we need and if people feel they're paying in but they're not getting things back then it obviously undermines the whole concept," he said.
"I don't think that's reached that stage yet - but it's something to watch out for."
He also expressed concern about health inequality.
"A combination of the impact of Covid, which will have affected the disadvantaged more, long waits for surgery which will affect people's ability to care for relatives or be employed and the opportunity for people to opt out of some of that and go private undoubtedly makes inequalities worse," he said.
Budget settlements for the coming years will inevitably have a bearing on the scale of future independent sector use by the health service.
Related topics
- Published27 September 2021

- Published6 January 2023

- Published30 December 2022
