Methadone programme 'is a black hole', says drug misuse expert
- Published
The dispensing of methadone has increased in a third of council areas despite an overall national decrease
The methadone programme in Scotland is "out of control", an expert has warned.
Dr Neil McKeganey, from the Centre for Drug Misuse Research, said "it is literally a black hole into which people are disappearing".
Data obtained by BBC Scotland showed pharmacists were paid £17.8m for handling nearly half a million prescriptions of methadone in 2014.
In response, the Scottish government said both doses and costs linked to opioid treatment had been dropping.
Community Safety Minister Paul Wheelhouse told the BBC: "Fewer Scots are taking drugs - numbers are continuing to fall amongst the general adult population, and drug taking among young people is the lowest in a decade."
However, a lack of data to measure the programme's impact was the focus of criticism from Dr McKeganey.
He said: "We still don't know how many addicts are on the methadone programme, what progress they're making, and with what frequency they are managing to come off methadone.
"Successive inquiries have shown that the programme is in a sense out of control; it just sits there, delivering more methadone to more addicts, year in year out, with very little sense of the progress those individuals are making towards their recovery."

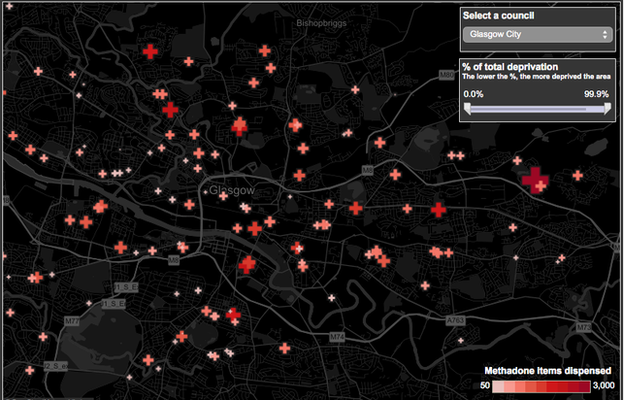
Use the INTERACTIVE DASHBOARD, external developed by BBC data journalist Marc Ellison to see how much methadone was dispensed near you in 2014.

But David Liddell, director of the Scottish Drug Forum, disputed claims that addicts were parked on the methadone programme.
He said: "What we know is the level of methadone being dispensed continues at the same level, but it's not the same individuals.
"Our sense is that of the 20,000-plus people on methadone, it will be less than half who are on it for a very long period of time."
However Mr Liddell admitted that, unlike England, there is currently no data in Scotland on whether users are relying on the programme indefinitely.
Regional increases
In 2013, pharmacies claimed back more than £17.9m from the Scottish government for handling 470,256 prescriptions of methadone - 22,980 prescriptions more than in 2014.
But despite this overall decrease, new data - obtained from National Services Scotland through a freedom of information request - revealed the number of methadone prescriptions has increased in more than a third of Scottish local authorities over the last two years.
The Edinburgh council area saw the largest increase in prescriptions (2,949), followed by Falkirk (421) and Argyll and Bute (405).
The largest decreases were found in Renfrewshire (5,842), Inverclyde (5,611) and East Ayrshire (5,598).

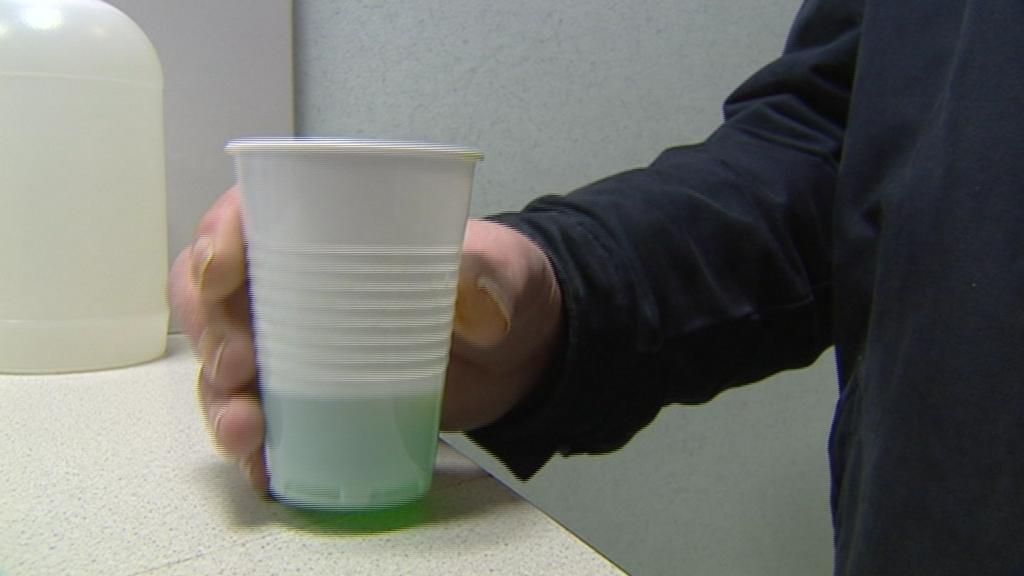
Methadone has been used to treat heroin addiction in Scotland since the 1980s
And while fees paid to pharmacies for dispensing methadone have declined over a four-year period, Dr McKeganey said the average annual outlay does suggest users are parked on the drug.
Dr McKeganey said: "The aspiration contained within the government's 'Road to Recovery', external drug strategy explicitly said that the goal of treatment must be to enable people to become drug-free rather than remain on long-term methadone.
"These figures show you that we are not achieving that goal - we are not witnessing large numbers of people coming off the methadone programme."
New strategy
Methadone has been at the heart of drug treatment strategies since the 1980s, but its use has been widely criticised by recovering addicts and drugs workers.
Methadone is by far the most widely used of the opioid replacement therapies (ORT), with an estimated 22,000 patients currently receiving it, but some users take it for years without being weaned off it altogether.
However a review commissioned by the Scottish government, external in 2013 concluded methadone should continue to be used to treat heroin addicts.
There are alternatives, including prescribing medical heroin, but many in the drugs field say the debate should move away from these to an examination of how the wider needs of drug users can be met.
Dr McKeganey said methadone does have a role to play in helping addicts wean themselves off heroin, but it should not be prescribed as widely as it is now.

An estimated 22,000 people are currently on Scotland's methadone programme
He said he would like to see a two-year reassessment implemented so that if the "highly addictive" methadone does not seem to be working for an individual, they can then either try the more expensive suboxone, or enter a drug-free residential home.
"That seemed preferable to me than leaving people on a methadone prescription for years - and then the worry is that you've turned your heroin addicts into methadone addicts."
Figures released by the NHS in 2012, external revealed that methadone-implicated deaths increased dramatically in cases where the individual had been prescribed the drug for more than a year.
Recent figures from the National Records of Scotland also reveal methadone was implicated in nearly the same number of deaths as heroin in 2013, external.

Case study
'The biggest habit I ever had'

David is clean now but was prescribed methadone for seven years. He said it was the most addicted he has ever been.
He said: "It's more addictive than the street drugs I was using because it was daily - it was constant, it was pharmaceutical and an unadulterated substance.
"I was very aware it was probably the biggest habit I ever had as far as being hooked on drugs."
He said he was accepting of what it was - a prescription to keep him off street drugs and stabilise his life.
"So I never really had any thoughts on whether I should be on it, or what sort of period of time I should be on it for," David said.
"And so one year became two years, two years became three and so on."
David said he also regularly used other drugs while he was on methadone.
He said: "But I did use a lot less than I would have, and I think I was maybe a lot safer than I would have been [had I not been on the methadone programme].
"It took away a lot of the need to make money [through crime] to fund the habit".
He said he likes the idea of the two-year reassessment proposed by Dr McKeganey.
"I like the idea of people having targets - if it's not working for you, we look for something else rather than just being left on it forever more."

'Methadone millionaires'
The methadone data obtained by BBC Scotland reveals how much each individual pharmacy claimed back in fees from the Scottish government.
Last year more than £102,000 was claimed by just one pharmacy on Glasgow's Saracen Street in Possilpark - an area ranked the third most-deprived in Scotland.
The largest claims were made by pharmacy giants Boots and Lloyds, who reclaimed £3.8m and £3.3m respectively from their hundreds of branches across the country.
The fees paid back to pharmacies are not only for the dispensing of methadone, but for oral hygiene services, and the services of a supervisor to ensure the dose is taken onsite and not sold on the street.
Pharmacies apply to enter into a contract with their health board to provide methadone services and must justify the need for such a service within that locality.
Pharmacists in Greater Glasgow are currently paid £2.16 for dispensing every dose of methadone and £1.34 for supervising addicts while they take it.
The fees are negotiated with individual health boards to suit local needs, and are lower than in England.
But a spokesman from Community Pharmacy Scotland dismissed the "methadone millionaire" tag, external placed on such pharmacies in the past by certain media outlets.
He said: "Methadone is an NHS prescription medicine and as such a community pharmacy is obliged to provide it when it has been prescribed for a patient by a GP.
"While community pharmacists are paid to administer the program, the income is far outweighed by the time, administration and difficulties that can often be encountered by taking on a role in this difficult area.
"The argument is not a financial one - but a health and social issue."
A statement by the Scottish government did not address the lack of data to prove the programme was enabling addicts to become drug-free.
However, Mr Wheelhouse said: "Both the number of items and the number of defined daily doses of opioid treatment have dropped steadily over the past five years and the cost of methadone is down 19% since 2010-11.
He added: "Independent experts advise that opioid replacement therapy is a crucial tool in treating opiate dependency. However, we believe it is important that there are a range of treatments available that suit the unique needs of individuals.
"Prescribing opioid replacement therapy is an independent decision for individual clinicians, in line with the current UK guidelines on the Clinical Management of Drug Misuse and Dependence."
- Published24 March 2015
- Published22 August 2013
- Published17 August 2012
- Published14 December 2010
- Published4 November 2012
