HIV in Scotland: Do you know the facts?
- Published
Comedian Scott Agnew uses his HIV diagnosis to confront myths about the virus
There is no comparison between 20th and 21st Century HIV, according to a leading public health body in Scotland.
Modern drug treatment regimens mean that HIV positive people have a normal life expectancy. An HIV positive person may, in fact, live longer because they require regular health checks.
Someone receiving HIV treatment can get to a stage where they cannot transmit the virus to a negative partner, even through unprotected sex.
However, the stigma which cloaks HIV still prevents people from getting regular sexual health tests and seeking treatment following a positive diagnosis.
There are also vulnerable social groups in Scotland who are disproportionately affected by HIV.
Stigma
George Valiotis is the chief executive of HIV Scotland
HIV Scotland said there was still more to be done to address the social, educational, economic and health disparities that prevent people from accessing and engaging in sexual health services.
It is estimated that 13% of people living with HIV in Scotland are unaware they carry the virus. A total of 42% of new cases in Scotland are diagnosed late.
Without treatment, HIV can still have a profound effect on a person's health and wellbeing.
George Valiotis, chief executive of HIV Scotland, spoke to BBC Scotland's Timeline programme about the reasons why HIV stigma can stop people from engaging in testing, prevention and treatment services.
"Treatment will stop them from being infectious"
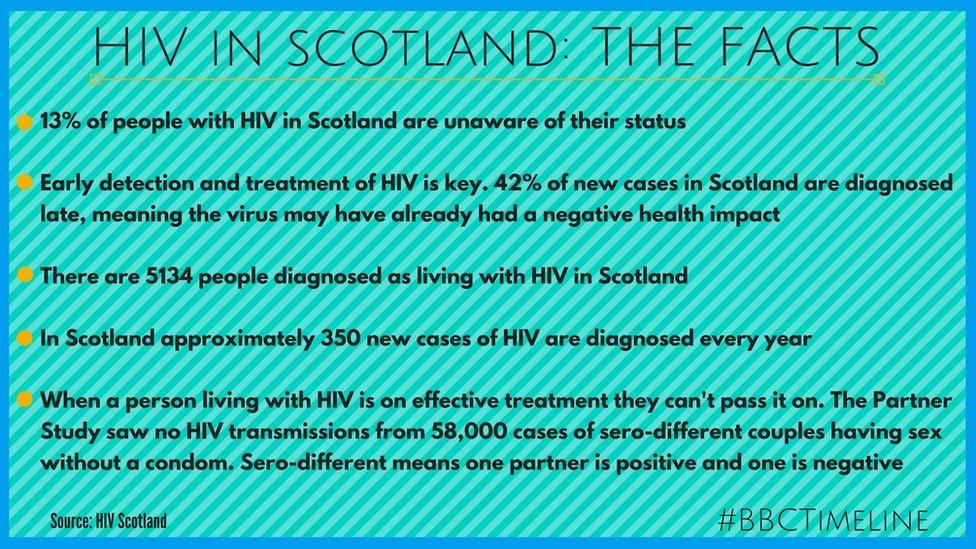
The facts about HIV
He said: "I probably don't even have to explain the fear that people have had about HIV over time and so that fear of being associated with this disease, which people also have a misunderstanding about, they have this dated idea about it."
"People have a 20th Century idea that it might be a terminal illness and so they are scared of being connected to that, they are scared over that being a possible future for them but we actually now know that we can treat HIV really effectively.
"So someone that is newly infected, put on treatment, will have a normal, healthy, life expectancy and also that treatment will stop them from being infectious.
"It really exiles people, that stigma, so we need to re-educate ourselves remind ourselves what HIV is now in today's age and therefore change our attitude about HIV."
Vulnerable groups
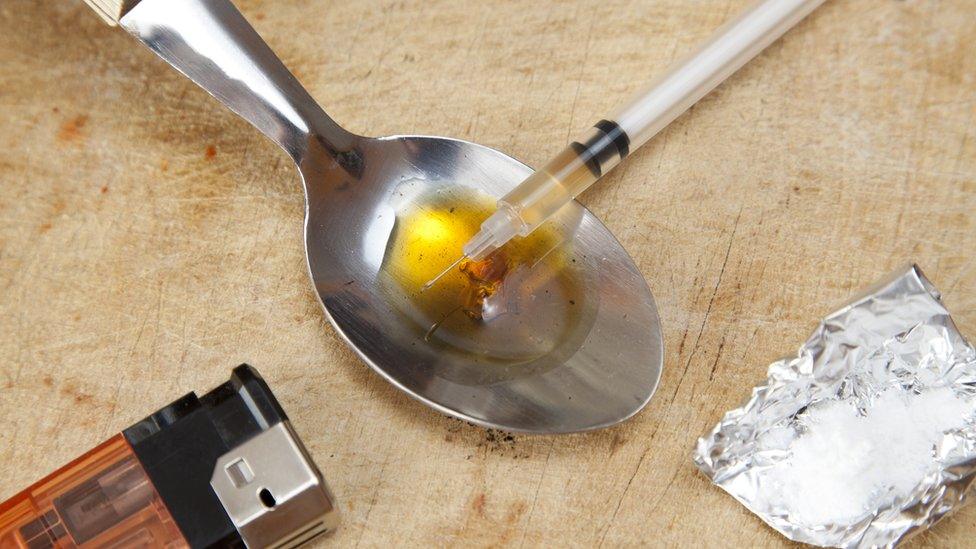
Injecting drug users are among the most vulnerable groups in Scotland who could contract HIV
HIV is still most prevalent amongst those who already face social stigma in Scotland. Gay and bisexual men, or indeed any other men who have sex with men, are still overwhelmingly affected by HIV.
Other vulnerable groups include people from black, Asian and minority-ethnic backgrounds. According to HIV Scotland, in some instances, the social structures of these communities can make negotiating condom use difficult and the stigma of an HIV diagnosis can make someone persona-non-grata within certain tight-knit groups.
Sex workers can also find themselves exposed to HIV due to the nature of their work.
And, while there is scant data available, HIV Scotland also reports evidence that transgender people are also disproportionately affected.
Intravenous drug use
Fiona contracted HIV through intravenous drug use. Now she fights to help improve drug laws in the UK
A former drug user, who now campaigns to reform UK drugs policy, has called for more action to help protect people from being criminalised through drug use and being disproportionately exposed to HIV.
Fiona Gilbertson contracted HIV when she was injecting drugs and describes herself as being in long-term recovery. Fiona says that stigma around addiction and UK drug policy leaves vulnerable people exposed to risks like HIV and criminality.
Fiona contracted HIV as a young woman
"We have such a stereotype of what IV drug use looks like," she said. "If I disclosed that to a medical professional they would assume that I was chaotic, they would assume that I was drug-seeking - not always, but I have had those assumptions."
Fiona says that heroin addiction should be treated as a health issue and that heroin-assisted treatment should form part of the answer to drug dependency in the UK.
"HIV is 100% preventable," she said. "I'm shocked and horrified to be sitting here 30 years on still talking about HIV outbreaks in Scotland. We are talking about an outbreak in Glasgow with one of the most vulnerable populations - homeless people.
"Unfortunately, because Scotland does not have power devolved to drugs policy we cannot make those decisions. Punitive drugs policy has no impact on drug use. There is vast international evidence on how you stop HIV outbreaks."

Fiona started Recovering Justice to look at the impact of drugs policy on problematic drug users
Fiona cites the Swiss model of heroin-assisted treatment, pioneered by former President Ruth Dreifuss, as an effective model to prevent people being exposed to HIV.
"She started a programme called heroin assisted treatment and she didn't do it in marginalised areas because she didn't want to stereotype people who use drugs as poor," Fiona said.
"Nobody has been infected with HIV, nobody has overdosed in a heroin-assisted treatment programme."
PrEP - Pre-exposure prophylaxis
Timeline spoke to three men who use PrEP to take control of their sexual health}
Another part of the HIV prevention toolkit is a drug called PrEP, which stands for pre exposure prophylaxis.
PrEP has been available on the NHS in Scotland since July. It is available, across the country, through sexual health clinics, subject to certain eligibility criteria.
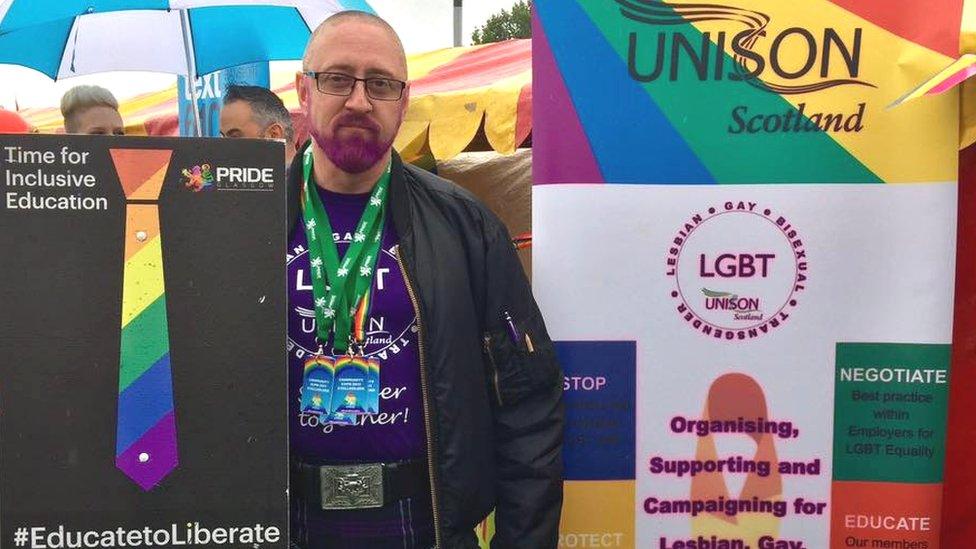
Watty Gaffney campaigns for equal rights for LGBT+ people
Watty Gaffney, a trade union worker living in Glasgow, has been taking PrEP since before it was available on the NHS.
"Since HIV became prevalent in the 90s there was a huge period where nobody actually spoke about sexual health, everybody was scared," he said. "And over the years as there has been better treatment and better advances in healthcare it's started to be something we talk about more frequently.
"I think HIV is one of these things that folk are concerned about discussing because they don't know how their family will react.
"They're concerned about how their friends are going to respond. There's a huge amount of stigma around HIV. A few of my friends are HIV positive and they've described it as they're having to come out again.
"I took it to protect myself"

PrEP has been available on the NHS in Scotland since summer 2017
"When I first looked into using PrEP, I bought it online," he said. "And that was something I took a very distinct decision to do. I had to know that when I was going out and meeting people, you didn't know their history, you didn't know how honest they were being with you and it's a decision I took to protect myself.
"When I started PrEP I was determined to make sure that people knew that this wasn't a bad thing, it wasn't a dirty thing. It was a protective mechanism that was in place that was just the same as taking the pill to stop you getting pregnant, taking anti-malarials when you go on holiday. Just a tablet every day and it just happened to be a tablet that stopped you catching HIV."
"PrEP is a really effective prevention tool"

First Minister Nicola Sturgeon is given an HIV test by George Valiotis, chief executive of HIV Scotland, at the Scottish Parliament, Edinburgh
George Valiotis, of HIV Scotland said: "Prep is a really effective prevention tool, if we can get it to the right people it means that it will stop them from getting HIV because when you take the PrEP pill, it stops you from being able to acquire HIV.
"If they keep taking that then that stops them from acquiring it and that overall reduces the total number of people with HIV each year.
"It's useful for anybody that's at high risk of HIV. People have often associated HIV only with gay men because HIV can be concentrated in gay communities but actually when we look at the HIV new infections, at any year in Scotland, it affects gay men, people who inject drugs, heterosexual people.
"So PrEP will benefit anybody that is in a high-risk profile."
HIV in the heterosexual population
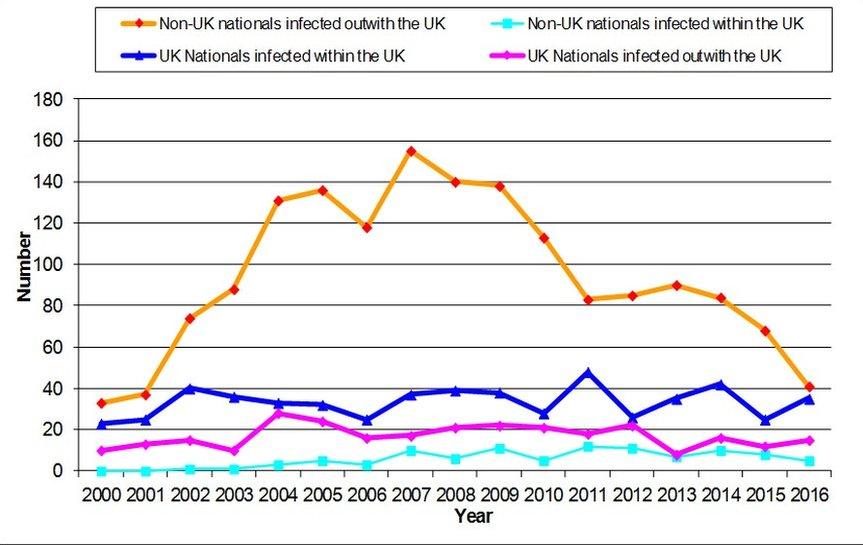
HIV rates among heterosexual people in Scotland
HIV does not discriminate by gender identity, race or sexual orientation.
A spokesperson from Health Protection Scotland said: "New diagnoses of heterosexually-acquired HIV have been decreasing steadily during the past 10 years - a decrease of 56% since 2007, reaching a total of 69 in 2016."
"This is predominantly in relation to those who have acquired their infection outside the UK in whom we have observed a 72% decrease in numbers with around 50 new diagnoses per year in the past five years.
"This is in contrast to a steady low number of diagnoses among those who have acquired their infection in the UK over the past 10 years and averaging 32 new diagnoses in the past five years.
"The most vulnerable could be considered to be those who have co-existing problems which may influence their behaviour for example excess alcohol use, drug use etc."
Further advice on sexual health is available by calling the BBC Action Line on 08000 680 675 or click this link. Lines are open 24 hours a day, all calls are free.
Timeline can be seen on BBC2 at 19:30 and later via the iplayer.