Is there an alternative to being parked on methadone?
- Published
'It was like I was sedated for 20 years'
Michael from Dundee spent more than 20 years on heroin substitute methadone. He felt like he was left constantly sedated, with no attempt to wean him off it.
"It suppresses every feeling, every emotion, your sense of sight, smell, everything," he says.
"Used in the right manner, I believe it would work but they are putting people on methadone and then just forgetting about them."

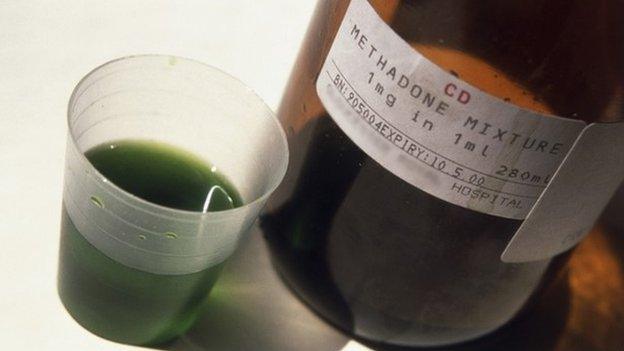
Methadone use was promoted in the 1980s to encourage drug users into the health system
The use of methadone increased massively in 1980s when health experts were faced with the problem of injecting drug users sharing needles, leading to a risk of spreading HIV.
The virus, which can lead to AIDS, was a new threat and, at the time, was untreatable.
Heroin substitute
Methadone, a heroin substitute in liquid form, was used to encourage drug users into the health system to give them care, advice and clean needles.
In terms of public health it worked, helping reduce HIV infection rates in places like Dundee and Edinburgh, which had the biggest problems.
Three decades later, more than a third of Scotland's 61,000 opioid drug users are on methadone.
Critics say some, like Michael, are effectively "parked" on the heroin substitute for years.
It is estimated that about 8,000 drug users have been on methadone for more than five years.
In addition it has been linked to a number of drugs deaths because some users continue to inject heroin while using legally prescribed methadone as well as illegal fake valium tablets.
So what's the alternative?
One is a relatively new treatment called Suboxone.
It is a combination drug made of buprenorphine which mimics the effect of heroin and Naloxone which blocks opiates ability to attach to the opioid receptors.
Michael has recently been switched from methadone to the more expensive Suboxone, which is used to taper users off drugs.
Eight weeks in, he can't believe the difference it has made to his life.
He says: "It's just astonishing how good it is.
"Now, life is like a drug. I just feel awakened. I'm here. I'm a member of society again."
But while Suboxone seems to be working for Michael, the drug does come with warnings of its own risks, side effects, and withdrawal symptoms.
Many experts say the debate should move away from alternatives to methadone to an examination of how the wider needs of drug users can be met.

Dave Barrie says the right solution has to be found for each individual
Dave Barrie, of the drugs charity Addaction in Dundee, says the important thing is to find the right way forward for each client.
If the "highly addictive" methadone does not seem to be working, someone may need a drug-free residential home instead.
There is also a debate about "fix rooms", where users inject heroin supplied by prescription under medical supervision.
Councillors in Glasgow claim the innovation will combat the increase in street injecting and HIV infections among users.
However, despite MSPs at Holyrood voting for the scheme, it can't get the full go-ahead because drugs policy is reserved to Westminster.
The Home Office insists its approach is to prevent drug use in communities and to support treatment and recovery.

Memorial garden at Addaction Dundee
Ten years ago the Scottish government published its national drug strategy, The Road to Recovery, with its main aim to get users drug free.
The next phase - the Substance Misuse Treatment Strategy - was meant to be published this spring, although that timetable has now slipped to the summer.

Dave Liddell called for some real blue sky thinking
Dave Liddell, of the Scottish Drugs Forum, says the time has come for some real blue sky thinking.
He says, even if Westminster blocks consumption rooms, new drug treatments, including one just approved in the United States, offer new hope.
Mr Liddell says: "I think it is an opportunity now, with a new strategy coming out fairly soon, to ask ourselves 'if we were starting from scratch, what would our services look like?'."
He says: "I think that is quite challenging when we have spent 30 years building them up.
"For example, there is a now a preparation which isn't licensed as yet in the UK, but which is a slow-release buprenorphine, where people would get an injection once a month.
"That would obviously mean that people would not have to attend a pharmacy on a regular basis."
And if recovering drug users can avoid having to go to a pharmacy every day for their prescription to be dispensed they can also avoid being preyed on by dealers as they run the gauntlet to and fro.
Michael in Dundee says: "I'm offered drugs every day where I go to pick up my prescription.
"I just have to say 'no, thank you, not interested'. They are so readily available.
"I could make a phone call now and get any drug I would want."
But Michael is 100% sure he will resist and stay on his new treatment.
"It's like I have been sedated for 20 years and I am actually coming out of it and finding life is great.
"It's lovely."
- Published20 April 2018

- Published5 April 2018
- Published25 March 2015