Drug-related Scottish hospital admissions highest recorded
- Published

Almost 8,000 people were admitted to hospital in Scotland in the year 2017/18 for drug-related reasons, according to new figures, external.
It is the highest rate of acute hospital stays recorded, and about four times higher than 20 years ago.
In total, there were 10,509 drug-related admissions - 90% of these due to a mental and behavioural diagnosis.
In 2017, it was estimated drug users cost about £100m per year in emergency hospital admissions.
The Information Services Division (ISD), which published the figures, said heroin and opioids were the most common cause of hospital admissions, accounting for 58% of drug-related stays, while approximately half involved people who lived in the most-deprived parts of Scotland.
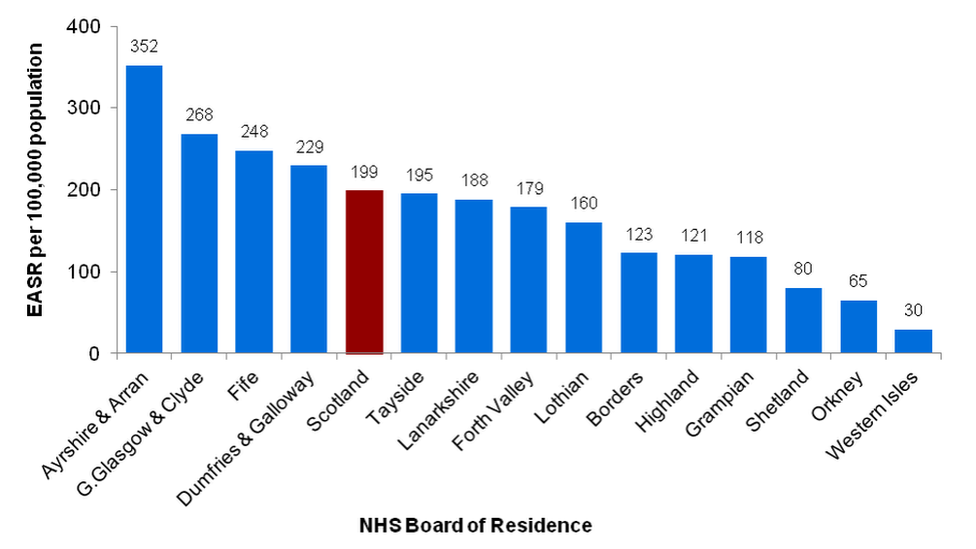
Drug-related general acute stay rates by NHS Board of Residence
Opioid use accounted for the highest percentage of stays in all but the oldest and two-youngest age groups, where almost a third (31%) of patients aged between 15 and 24 involved cocaine and 28% were due to cannabis-based drugs.
Almost all (95%) of drug-related hospital stays were emergency admissions, but ISD said most stayed in hospital for less than a week.
'No simple solution'
Drug-related stay rates varied by health board, with Ayrshire and Arran's NHS having the highest proportion of hospital stays because of drugs, with 352 stays per 100,000 of the population.
It was followed by Greater Glasgow and Clyde with 268.
Rates in rural Scotland were lower, with Shetland, Orkney and the Western Isles having the fewest admissions as a proportion of their populations.
Responding to the release of the figures, Public Health Minister Joe FitzPatrick said: "There is no single simple solution to addressing the harm caused by drugs.
"We're taking forward evidence-based actions and examining how services can evolve to ensure that they find those people most in need.
"This renewed focus has been backed by additional investment of £20m in drug and alcohol treatment and support services and will be used to improve the provision and quality of services."
- Published21 May 2019
