NHS crisis: 'Human tragedy' of patients waiting for surgery
- Published
Dr Caroline Whitworth said bed occupancy was now consistently at 100%
The number of patients waiting indefinitely for NHS surgery is becoming a "human tragedy", a senior doctor has told BBC Scotland.
Dr Caroline Whitworth, of Edinburgh Royal Infirmary, said bed occupancy was now consistently 100% with "thousands" in pain while on hold for procedures.
A&E waiting times have been at record levels since mid-August.
Most health boards have cancelled routine operations to make space for Covid patients and the seriously ill.
Bed blocking has also been an issue for the ERI, with over 100 elderly patients waiting to be discharged in recent days.
'Busiest in 20 years'
Dr Whitworth, a kidney specialist and medical director for acute services at NHS Lothian, said they cannot move patients fast enough to take more urgent cases in - largely because of hold-ups in social care.
"I think the hospital is the busiest I have seen it, and I have been a consultant for over 20 years," she said.

Staff at ERI are facing their busiest period in 20 years
"We wake up every morning to no free beds, and consequently a queue of patients waiting to come in, mainly from the emergency department.
"Some of those beds are closed because of staffing issues - staff who are unwell because of Covid or perhaps isolating because of Covid - and a very small proportion of beds are closed because of infection control.
"But over 80% of them are beds we cannot use because of patients who do not need to be in hospital but are waiting for that next step of social care."
18-hour waits in A&E
A&E staff at the Edinburgh hospital are now regularly dealing with 400 patients a day, when they used to see around 300.
Dr Dave McKean, who runs the department, said the number of patients does not tell the whole story, because they are seeing fewer people with minor injuries.
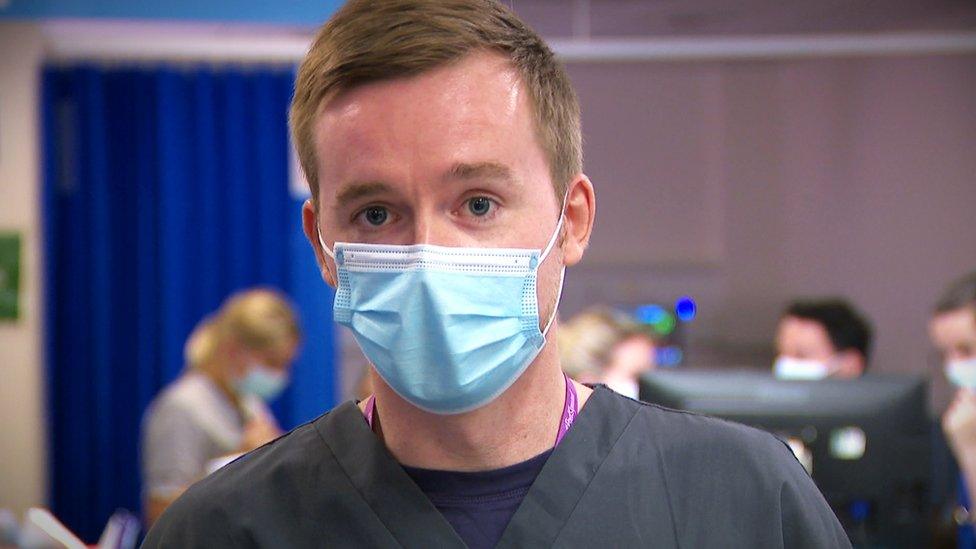
Dr Dave McKean said people are coming to A&E with more severe conditions
"That entire increase is all people with what we'd call major presentations," he said.
"So these are all people who need more investigation, they need more treatment and more of them need admitted to hospital.
"We are already in excess of what we would expect for a normal winter and we are barely into autumn."
The department has also seen a dramatic rise in the length of time people have waited for a bed in the main hospital.
Staff said it was not unusual for A&E patients to wait 18 hours - and those waiting take up the majority of their cubicles.
Problems in elderly care
This week, the hospital had more than 100 elderly patients waiting for transfer to their own home or to rehabilitation beds - which meant about one in 10 beds were taken up by such delays.
Staff managing beds for elderly care find the demand in acute hospitals is the same across primary care and community services, blocking the movement of patients through the whole system.
It is a problem across Scotland, with the social care system struggling to keep up with the needs of elderly patients who require support to leave hospital.
The average number of beds taken up each day in August by delays to patients being discharged was 1,489.
For other patients, often waiting in pain for elective (or non-lifesaving) surgery, the knock-on effect of Covid and bed shortages is that there is no end in sight, according to Dr Whitworth.

A&E staff at Edinburgh Royal Infirmary are anxious for the coming winter as waiting times dramatically rise
She said: "We are trying very hard to increase the capacity, but our theatres can only run at two-thirds of normal capacity because of the infection prevention and control measures, and without those extra beds that we need to bring people in, that's our limiting factor.
"It is having an enormous impact, and the human tragedy arising from that, we recognise. We have thousands of patients waiting for surgery, but at the moment we are having to prioritise those patients who have really serious illness, cancers for example or other needs for surgery which has to be done as soon as possible.
"But it means that other patients perhaps waiting for hip or knee replacements will perhaps be waiting for a very long time."
The winter ahead
On Tuesday, Health Secretary Humza Yousaf promised £300m was to be spent on 1,000 new NHS support staff, as well as increasing pay for carers and more beds in step-down facilities.
Dr Whitworth believes the money could make an "enormous difference" if it was used for social care needs, as it would free up 15% of beds that could be protected for surgery.
However, she said the need for staff to be trained means progress will take time.
Meanwhile, teams across this huge hospital are trying to prepare for the busiest time of year - with no slack in the system.
Staff are apprehensive, and have urged people to "think twice" about how they use the NHS services this winter.
Related topics
- Published22 July 2021

- Published23 September 2021
