Why we should worry about what is happening in A&E
- Published
- comments

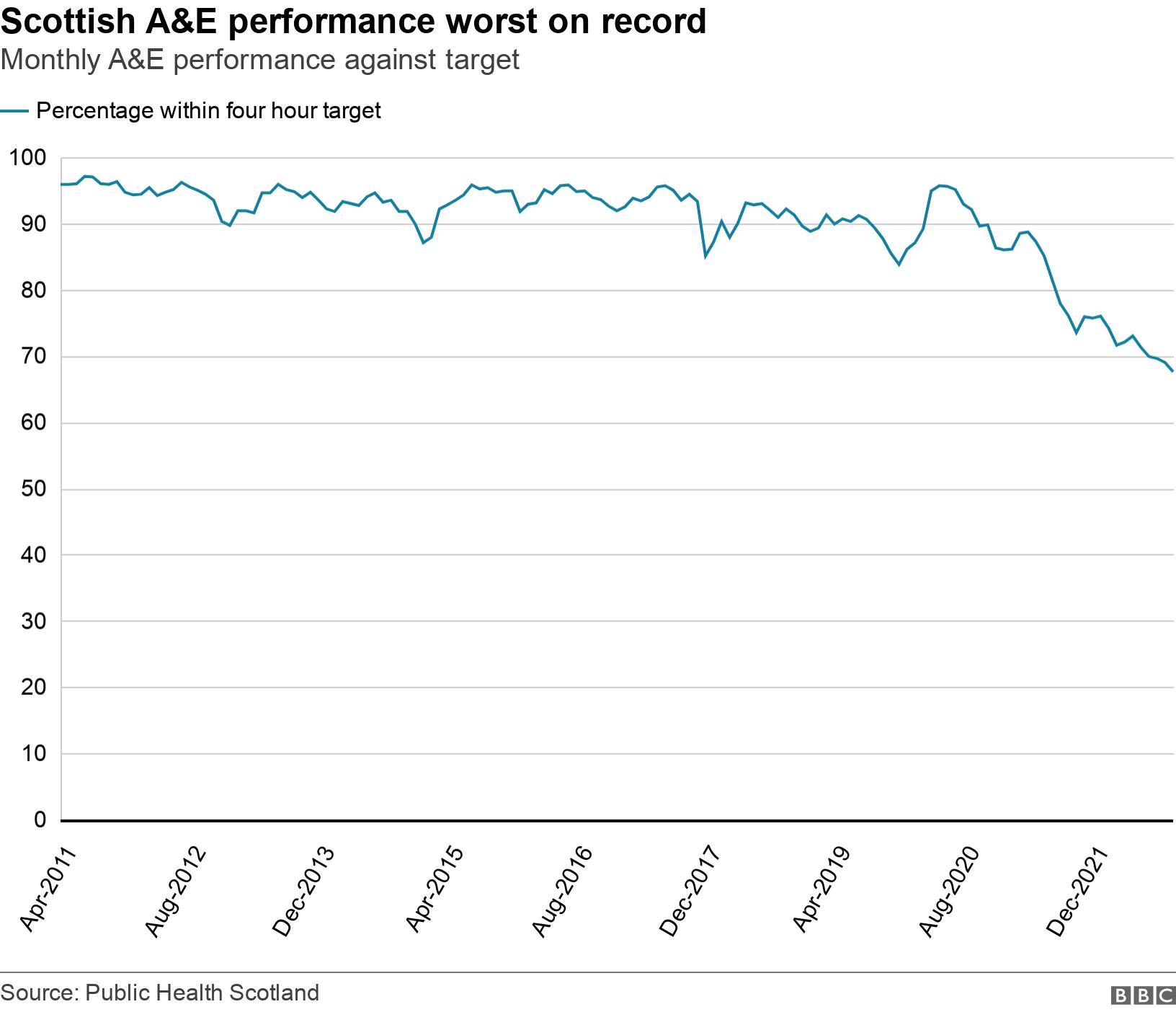
The latest A&E waiting time figures are once again the worst on record.
In the week ending 27 November just 61.9%, external of patients attending emergency departments were dealt with within the four-hour target.
And the problem is far more acute at Scotland's busiest A&Es.
The crisis in A&E shows what is happening across the whole system.
Separately, the number of hospital beds occupied by people who are medically well enough to go home, external is also at a record high.
This means patients can't get into hospital because there are no beds and they can't get out because there is not enough social care.
The pressure this causes seeps into every single part of the system.
Staff are stressed and burnt out while patients are at risk because they can't access the care they need.
It is pretty obvious that when you are very ill, waiting for a long time in an emergency department is not a good idea.
You only need to look at social media to see regular posts from A&E staff who describe how stressful and dangerous they feel things are.
I get regular calls from emergency medicine doctors telling me they are in despair and can't cope with the relentless demand.
One consultant told me that they are taking more and more risks.
They say that having ensured a patient is not facing a life-threatening situation they are making the call that it is probably better to send them home to follow-up with their GP.
The alternative could be the patient languishing on a trolley in a brightly-lit corridor for many hours before a bed becomes free.
In Glasgow, doctors who feel they cannot speak publicly have talked me through the pattern of their daily handovers. They say phrases such as "an unsafe environment", "no available resus (resuscitation) beds" and "patient's life is at risk" are routinely documented.
These doctors say they have seen patients die simply because they could not get to them in time.
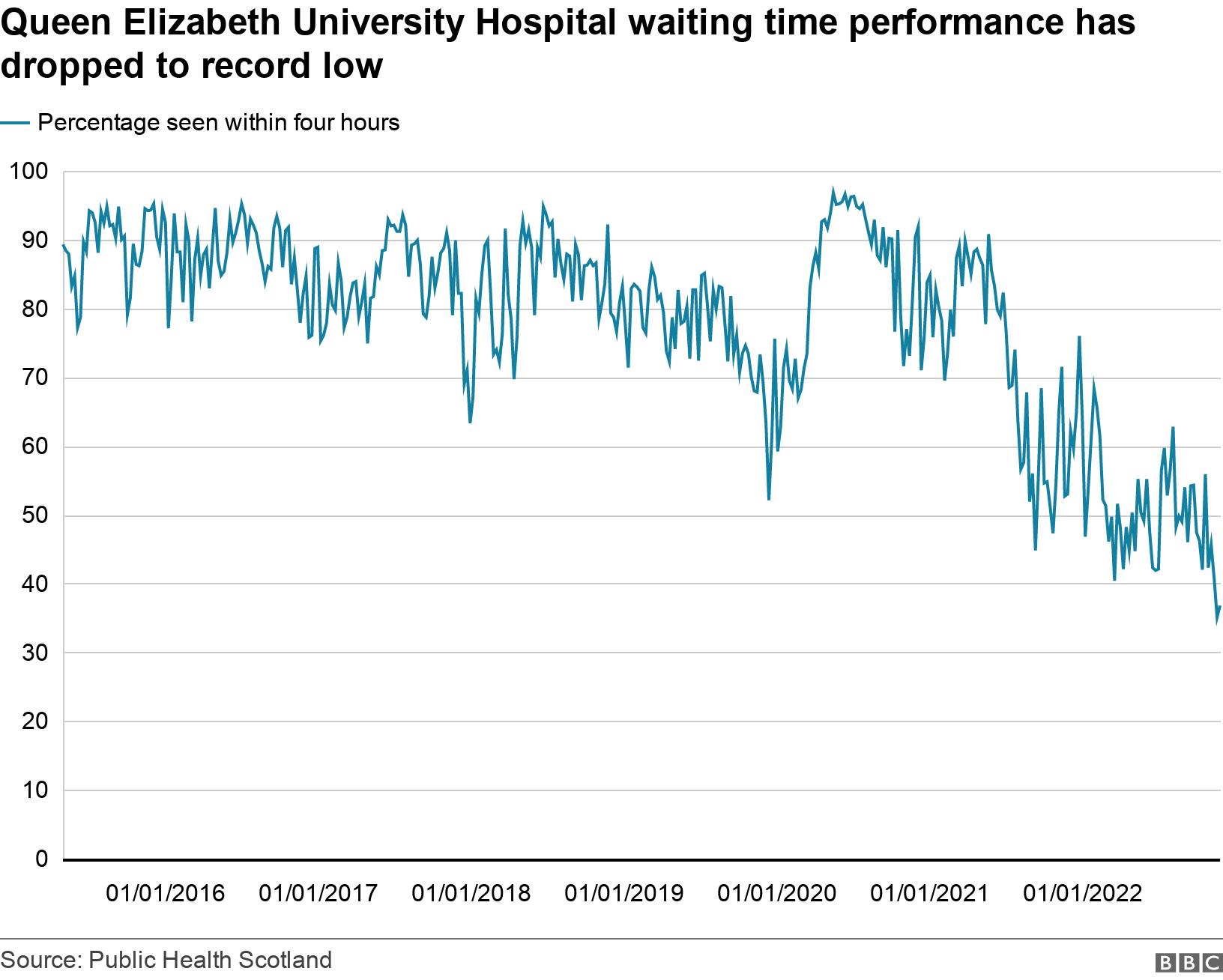
Last week the Queen Elizabeth University Hospital (QEUH) in Glasgow recorded its worst ever performance for A&E. Only 35.1% were attended to within four hours. The latest figures were only slightly better.
Scotland's busiest A&E - Edinburgh Royal Infirmary - and Forth Valley Royal near Falkirk have both had more than six out of every 10 patients waiting more than four hours.
Some days were even worse than the stats show.
A performance chart shared with me shows that at the QEUH, on Saturday 19 November, of 233 patients who showed up at the emergency department, only 21.9% of patients were seen within the target time.
One internal document I have been shown makes reference to 11 ambulances queued outside the hospital when there were no available spaces in A&E, which was four nurses and a consultant down.
Some of the proposals outlined to stop ambulances getting stuck outside the hospital include offloading patients into corridors.
One doctor spells it out - if this was an operating theatre, the staff would simply not be allowed to carry out surgery because it is not safe. But A&E can't close.
"There needs to be a full inquiry into what is happening in our emergency departments," they say.
The Royal College of Emergency Medicine (RCEM) has long said that delays in A&E lead to people dying unnecessarily.
It carried out research that suggests there could be one avoidable death for every 72 patients waiting between eight and 12 hours in A&E.
The latest monthly figures show that in October, external there were 15,467 patients who waited more than eight hours.
There were 6,814 who waited more than 12 hours.
Both of these figures are record highs and, according to RCEM calculations, could be resulting in as many as 200 avoidable deaths in a month.
What is the problem?
Last month the BBC revealed documents that showed senior health board leaders were concerned unscheduled care was "going to fall over in the near-term before planned care falls over".
Minutes of a meeting of Scotland's NHS leaders in September show ideas on how to address this include discharging people from hospital after 23 hours.
They point to data that indicates the NHS is not actually overwhelmed, with the number of people arriving at hospital not radically different to any other time.
The real issue, they say, is delayed discharge - getting people home when they no longer need acute hospital care.
But to fix that requires a radical improvement in social care and access to community health care.
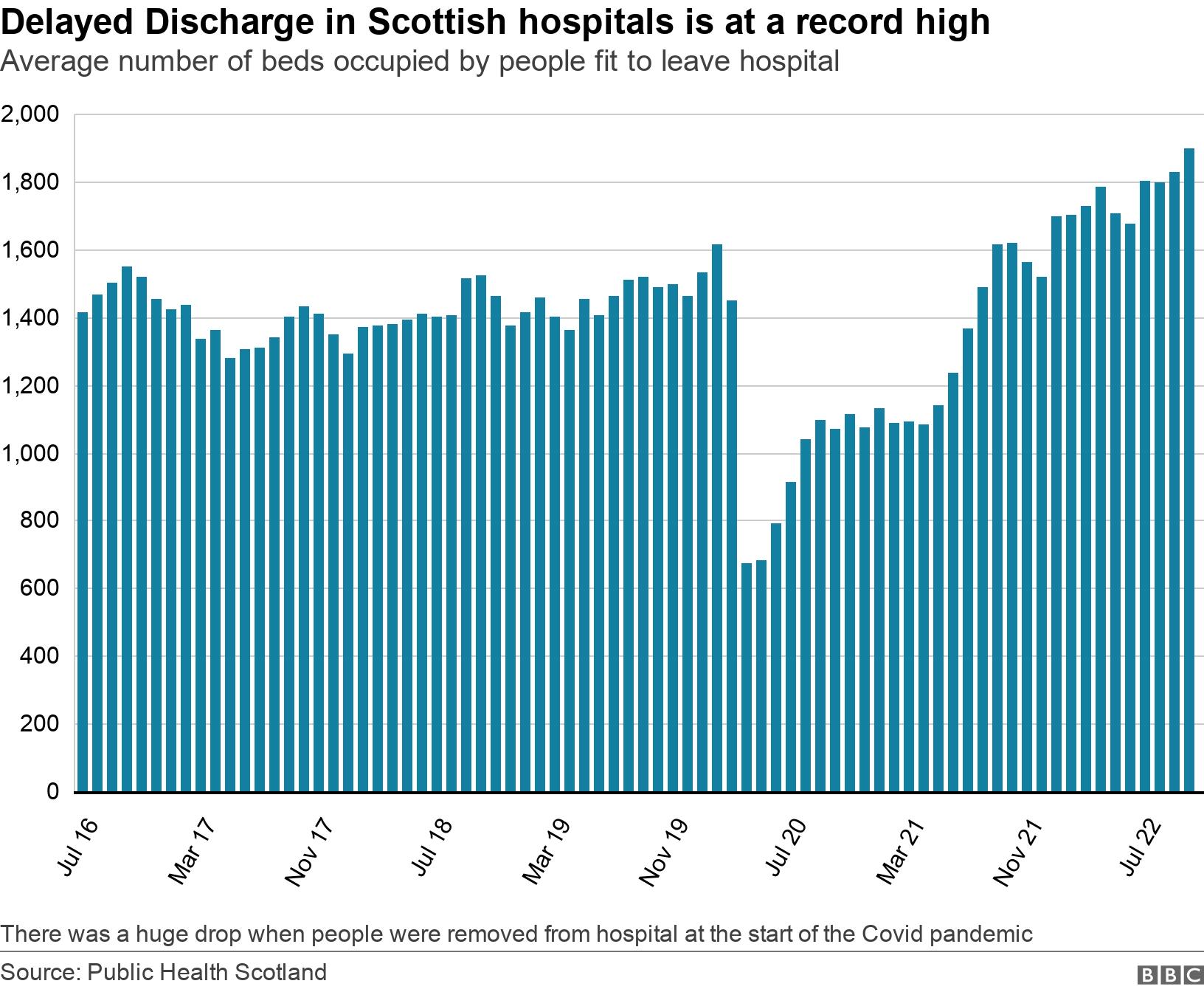
The latest delayed discharge figures, external show that in October the average number of beds occupied by people who no longer need hospital care was 1,898, the highest figure since the current guidance came into place in July 2016.
As many as one in every six beds in a hospital is occupied by a patient who is medically ready to go home but can't.
Of course it is not always straightforward to discharge patients who no longer require treatment in hospital. They may need major adjustments to their home if they can no longer manage stairs, for example, or need carers to help them dress, shower or eat.
One doctor in Lanarkshire told me that things are so bad now, they can assess a patient on one shift and come back 24 hours later to find that same patient still in A&E waiting for a bed. That is despite the board adding extra beds into wards to try to increase capacity in their hospital to admit new patients.
As I said at the start, what is happening at A&E reflects the health of the whole system.
A nurse working in Edinburgh told me there can be many tears on a shift but staff support each other, pick themselves up and get on with the next shift.
Patients are deeply frustrated they can't get through to their GP, or spend hours on the phone after dialling 111 - so they end up at A&E.
Meanwhile health boards continue to call for patients to avoid coming unless it is a life threatening emergency.
None of this shows signs of getting any better, any time soon.
Related topics
- Published29 November 2022

- Published21 November 2022

- Published1 November 2022
