Covid in Scotland: No more 'easy wins' for hospital staff
- Published

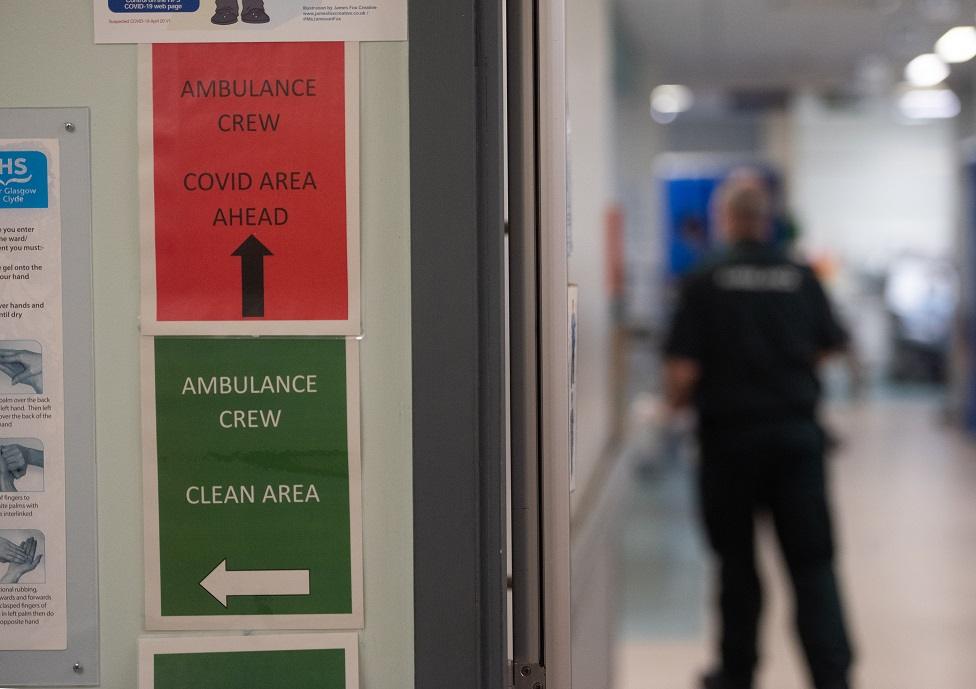
The emergency department at Glasgow's Queen Elizabeth University Hospital is the biggest and busiest in Scotland.
Ambulances keep arriving, bringing more patients. In a curtained cubicle, one man is explaining to the doctor that he's been in pain for days, but he put off coming in "because of everything that's going on".
Dr Alan Whitelaw, who runs the department, says that while there might be fewer patients coming through his door, there are no longer any "easy wins".
"Those that are coming are the sick people," he says. "We are undoubtedly seeing the effects of people not seeking healthcare for six to 10 months.
"We are seeing disease that we wouldn't always see and we are seeing it further down the road.
"We are making more diagnoses that potentially would be made in primary care or outpatient clinics. On top of that we've got lots of Covid patients coming through the door.
"So it is those two things together that currently put the NHS under that significant pressure."
All over Scotland, hospitals are under severe pressure, with some treating significantly more coronavirus patients than they did during the first wave of the pandemic.
Public visitors are not allowed at the QEUH, but BBC Scotland was given special permission to film to highlight the impact of Covid and the importance of following lockdown rules.

On the day of the BBC's visit, there are 244 Covid patients. Critical care is running at capacity, and across the whole hospital it's a constant challenge to find space for new patients.
Dr Whitelaw says the level of unpredictability is extreme. His team has run out of spare beds.
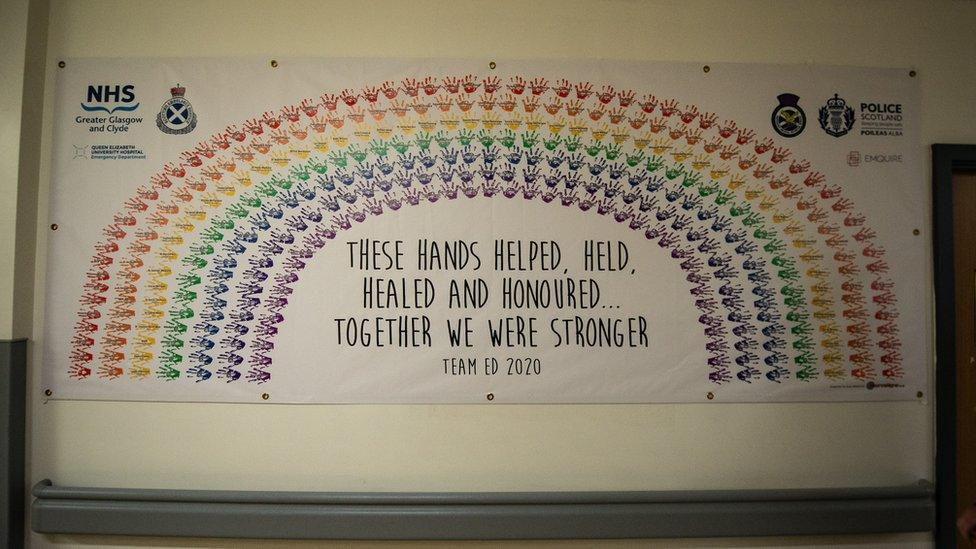
"We are ten months into strange and difficult times. It's winter, no-one's had a holiday, no-one's had much downtime.
"Hospitals are fuller in winter, beds are tighter and patients are sick".

Upstairs, one ward that previously treated patients with infectious diseases like flu or norovirus, is now a Covid ward. All 28 beds are full.
Some patients here are recently diagnosed, others are coming to the end of their isolation, while some have been stepped down from critical care, but need rehabilitation.
Senior charge nurse Karen Paton says it feels like patients are now sicker for longer.
"We've had this going on for more or less a year now and staff are beginning to feel the emotional distress of it," she says.
"Having to deal with patients succumbing to coronavirus, and just having the emotions of all the patients not being able to have contact from their families.
"I think it's beginning to take its toll on everybody."

Covid patient Gerry Gilroy says QEUH staff have been "superb"
In one room on the ward is Gerry Gilroy, who tested positive for Covid in late December. By 8 January, the day of his 66th birthday, he could barely get out of bed and couldn't eat.
"It just hit me and I knew there was something not right," he says.
"I know how serious it is. I never thought it would hit me. It's been a bit of an experience but thankfully I'm on the mend.
"The staff here are superb. When I get out of here, if I can do something for the NHS I'm going to. Doctors, cleaners, nurses, all top drawer."
The impact of Covid is being felt across the hospital. The acute receiving area used to be the first stop for people who needed urgent surgery.

Now it's where medics like Dr Colin Perry assess Covid patients sent in by their GP or NHS 24. It's another area that's full.
"In the first wave our ICU was busy and it remains very busy, but during that period we had free beds," says Dr Perry.
"This time we have much more pressure on the downstream ward areas, so it is harder to manage the wider needs of the hospital and make room for patients to move through the system.
"The numbers are far higher than they were a year ago."
Repurposing so many wards to treat coronavirus patients has meant some routine work had to be postponed, but staff are working to prioritise all different kinds of treatment.
Helen Dorrance is a senior surgeon who specialises in bowel cancer at the QEUH. On the day the BBC visits she is operating on patients from another hospital to help relieve pressures there.
Demand for critical care makes it difficult to operate some services, but cancer treatment is still running.
"We work together as a team across the region to make sure people who are the highest priority get dealt with," she says. "But everyone gets their fair share and access to the care they need.
"It's not a choice, we do have to provide the best care we can for Covid patients and my critical care colleagues are stepping up to the mark.
"But the rest of us are making sure the rest of the service runs the way it should, so if you have your heart attack or stroke the right people are there to give you the best care."
Coming to hospital for any reason during the pandemic is a different experience, and services are stretched.
But the emergency department's Dr Whitelaw adds that no matter what happens, they will cope.
"We don't come to work to worry or be fearful, we come to work to do our best and to help," he says.
"I think there's an uncertainty about what the next two to three weeks look like.
"It might be very, very challenging but I have absolute faith that the staff here will continue to do everything that is required.
"I think the public should be reassured that no matter what is thrown at us we will definitely get through it."


- Published20 January 2021

- Published20 January 2021

- Published13 January 2023
