Covid in Scotland: A&E staff fear post-Christmas rise in virus cases
- Published

Staff at Monklands Hospital in Airdrie are working at full capacity
Doctors treating Covid patients in Lanarkshire say they expect to see a further rise in hospital admissions after Christmas - but they hope it won't be "another huge spike".
Staff working in the infectious diseases ward at University Hospital Monklands also told BBC Scotland that vaccinations were playing a critical part in stopping the health service being overwhelmed.
More than 100 coronavirus patients are currently being treated across NHS Lanarkshire's three acute hospitals, compared to more than 350 during the January peak.
But the site at Monklands is working at full capacity and emergency medics admit they are struggling to meet demand.
For example, every week since the summer more than a fifth of A&E patients have waited longer than the four-hour target.
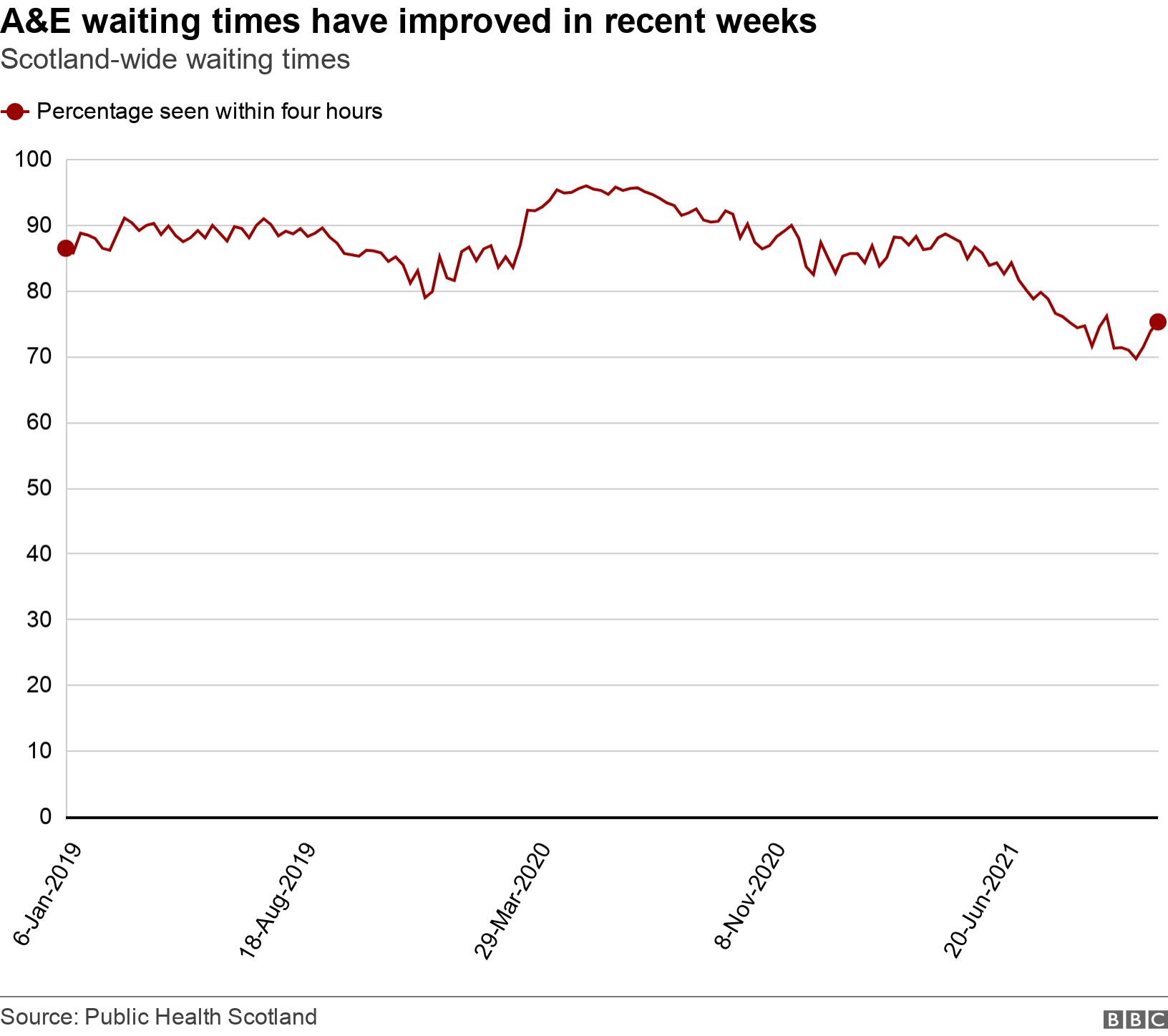
The latest figures from Public Health Scotland, external show that 75.6% of patients at Monklands emergency department were seen within four hours in the week up to 14 November.
The figure is down from 78.3% the previous week.
However, only three of Scotland's 30 hospitals are currently meeting the target of 95% of patients being admitted, transferred or discharged from A&E within four hours.
The figure for the whole of Scotland is 75.2% - an increase on the previous week.
Patients waiting in cars

Dr Fiona Hunter said medics want to be able to treat patients in a "timely manner" but are being "overwhelmed"
Dr Fiona Hunter, who runs the department, described the workload as relentless.
She said: "It's unprecedented pressure, unprecedented demand.
"We have patients that have to wait in cars. We just don't have the room for them.
"We really are not here for anything and everything, we are here for emergencies and we want to be able to see the sickest patients first and in a timely manner and we can't do that when we are overwhelmed by patients."
Dr Hunter also conceded her staff cannot offer the level of care they want to due to the pandemic.
She added: "We used to be a well-performing site in terms of meeting the national figures, and now we are one of the poorer sites, and if you compare that with the number of Covid patients in Lanarkshire, I think you'll find there is a link there and we can't continue to see the amount we are seeing."
Almost all of the available beds in the hospital are occupied and about 15% of them are currently taken up by virus patients.
In the infectious diseases ward, they account for about half of the total.
'Young people becoming critically unwell'

Specialist consultant Dr Nick Kennedy said getting the right patient to the right bed is a problem
Last year the ward saw an endless stream of elderly patients who ultimately deteriorated and died.
This winter specialist consultant Dr Nick Kennedy said those being treated are typically younger and responding well to treatment.
He added: "Nevertheless, it is a bit of a wake-up call if you're in your 30s, 40s or 50s because people are still ending up in hospital.
"We are still seeing young people becoming critically unwell and even ending up in intensive care."
He worries that it ultimately compromises patient care elsewhere.
Dr Kennedy said: "An older hospital like this lacks side rooms, so it's trying to get the right patient into the right bed.
"One always manages one way or the other, and one always prioritises the acutely ill patients that come in the front door and they always get seen and they always get care.
"But we want to provide excellent care, never mind good care, and that's the challenge."
He said that following a spike in hospital admissions in September, case numbers have levelled off for now.
But looking ahead, Dr Kennedy warned: "My personal prediction would be that the next few weeks won't be too bad, but we are very apprehensive about what happens after Christmas and into the new year.
"People will be gathering, and there are lots of reasons why we can anticipate that community transmission of Covid will increase and we are anticipating that we will have an increase in the number of hospital admissions in the new year period.
"Hopefully not to the extent that we had last year. Hopefully it will be an increase rather than a huge spike."
'We're already broken'

Dr Katie Sykes described last winter as "terrible"
Dr Katie Sykes is another infectious diseases consultant at the hospital. She said the ward has had to remain very flexible as the demand for high-dependency care has risen and then shrunk back.
She admitted: "On a daily basis we don't really know what's coming next.
"We're in a difficult situation. Covid is still there and we've got flu that may come later in the winter and we don't know how big the flu epidemic will be this year."
Dr Sykes is genuinely worried about what could lie ahead.
She said: "We're approaching this winter in a state where we're already broken. We've been working in crisis mode for nearly two years and there's a limit to how far people can go. They're really having to dig deep now.
"Last winter was terrible but we worked as hard as we could to deliver the highest standard of care we could.
"I think we'll do it again but there will be a cost, and probably that cost will be the wellbeing of staff, our family lives, our relationships and our lives outside work are probably going to suffer, but we will get through the winter."
'It definitely won't be a normal Christmas'

Charge nurse Kerry Reid said staff will not have a normal Christmas
Dr Kennedy said staff feel vaccinations are a critical part of stopping the hospital from being overwhelmed.
He continued: "Although you know quite a number of people who get vaccinated do end up in hospital, what you don't see is all the people who don't end up in hospital. You've got about a 90% protection.
"Even if you do end up in hospital, you're unlikely to get as sick and you're unlikely to die and we feel much more positive as clinicians that we're going to have a good outcome if a patient is vaccinated."
He said even small increases in vaccine coverage of the population would make a difference to the pressures they are facing as they head through the next few months.
Charge nurse Kerry Reid said they all know there won't be much time to celebrate over the festive season.
She recalled last year was "really hard" and added: "Everyone's tired, missing out on family time, everybody's life's been put on hold for a long period.
"For nursing staff and medical staff it definitely won't be a normal Christmas."

