Organ donation: Views from the frontline in Cardiff
- Published

Transplant operations in Wales only take place in Cardiff with organs coming from across Wales and other parts of the UK
Wales has become the first UK country to introduce a soft opt-out system for organ donation.
From Tuesday, the assumption will be that people are willing to donate unless they opt out of the process.
The University Hospital of Wales in Cardiff is the only hospital in Wales where pancreas and kidney transplants take place.
In the year to April, surgeons here transplanted 183 organs from 57 donors, external - benefiting 141 patients.
Around a third of the organs came from patients who had died at other hospitals in Wales.
There are hopes of increasing the number of donors with the new legislation.
Medical staff involved in the process have given their views on the change in the law - and a patient who had just received a kidney in a transplant operation.

Dr Graham Shortland says it is important everyone is informed and the results of the law change are evaluated
Dr Graham Shortland, medical director, Cardiff and Vale health board.
"Perhaps we'll be dealing with an extra 15 donors a year; but let's reflect. From one donor we will have a number of organs donated - kidneys, liver and the heart - which can be used in different ways," Dr Shortland said.
"It can add to the pool of donors which can be used for patients who require transplantation. But there's also an important message around increased awareness of organ donation as a whole."
Dr Shortland said the unit was part of a UK national network for safeguarding the use of precious organs to ensure they are used in the best and most efficient way.
He said the hospital had also worked on increasing capacity, developing a post-anaesthetic care unit, to give patients high-level care and close monitoring after surgery before they go back to the ward.
"We've reduced the number of cancellations significantly that we're getting for major surgery - cancer surgery and other types of surgery."
It was important to ensure the population was informed and how the outcomes for transplantation and patients from the changes in the law were evaluated, he added.

Consultant Dr Chris Hingston explains to Owain Clarke the difference the change in the law will make
Dr Chris Hingston, consultant in intensive care medicine and regional clinical lead for organ donation in south Wales.
He said working in intensive care was about saving lives but 20-30% of patients would not get better.
For heart, lung, kidney and liver donation to take place, patients have to be brain stem dead and on a ventilator and two doctors need to agree that further treatment is futile.
Dr Hingston said families played a key role and they "would never force anyone" to agree to donation in what was a stressful time.
"With the conversations with families, all we want to do as clinicians is to make a choice they're comfortable with and above all respecting the last known wishes of the family member," he said.
"People might have changed their mind. We need information to know if they lived in Wales, medical information to ensure transplant is as safe as possible - it's not without risk - and we need to know the last known wishes. "
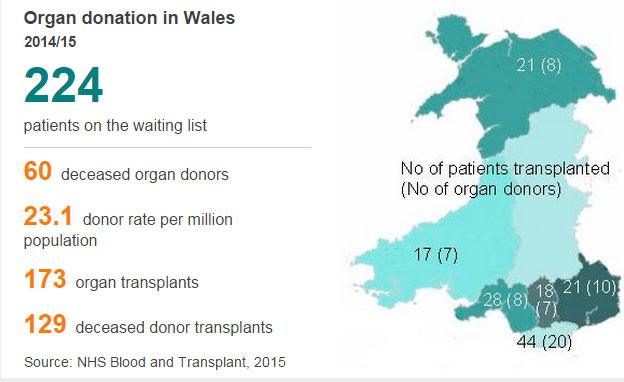
Organ donation in Wales
2014/15
224
patients on the waiting list
-
60 deceased organ donors
-
23.1 donor rate per million population
-
173 organ transplants
-
129 deceased donor transplants
He said he was confident that the system would be able to cope.
"We need to have the equipment, the staff, not just the organ donors; it's the whole package. The projected figures are for an extra 15 donors a year - that's at least 45 organs available across the UK.
"But we have to remember those 15 donors will be spread out across a large number of hospitals across Wales."

Transplant surgeon Mike Stephens says even a small increase in donors could make a big difference to people's lives.
Mike Stephens, transplant and organ retrieval consultant surgeon.
"It's frustrating seeing patients waiting long periods of time and even more seeing their health deteriorate during that period," he said.
"A number deteriorate to the point when they're not well enough for a transplant.
"That's really a shame and the reason for that is we don't have enough organs."
He said although the rise in donor numbers might be small, the number of patients to benefit would be far greater.
Mr Stephens said he could understand family caution but said the conversation about what to do in the event of their deaths could be had earlier, at a far less traumatic time.
"You have to have this as a discussion that we're comfortable with. No-one likes talking about death. But we're trying to encourage people to think about it, what their wishes are if they were in that position and let their relatives know."

Specialist organ donation nurse Angharad Griffiths explains her role with families
Angharad Griffiths, specialist nurse for organ donation, involved in liaising with families.
"The conversations we'll have will change slightly. From 1 December, everyone in Wales has the opportunity to become an organ donor [currently one million people registered] and they can now register not to be a donor [around 86,000 to date]," she said.
"If they choose to do nothing, then we will approach families with a slightly more presumptive approach.
"Unless there was absolutely no idea what that patient felt about organ donation, that's the only time we'd then start to talk about deemed consent. We would assume the patient had no objection to organ donation."
She said it was not about imposing legislation but talking with the families and not putting them under any more distress than they were already under.

Kidney transplant patient Calvin Jones describes what it was like after his organs started to fail
Patient Calvin Jones, from Carmarthenshire, has just had a kidney transplant in Cardiff after being on the transplant list since June 2014.
"I was on dialysis from March of last year and I had no life really, my kidneys had finished," he said.
"With this change in the law, it will save a lot of lives, and also it gives people a form of life, they can live an extra 10 or 15 years to do naturally what they do every day."
- Published1 December 2015

- Published30 November 2015

- Published6 October 2015
- Published23 August 2015