NHS Wales urged over cancer diagnosis change
- Published

Health experts from Wales being shown a diagnosis centre in Aarhus, Denmark
NHS Wales can be among the world's best for cancer care if big changes are made in how quickly it is diagnosed, says an international expert.
Wales and the other UK nations have some of the worst cancer survival rates in the developed world.
But Prof Frede Olesen said lessons can be learned from Denmark, which has improved how patients with less obvious symptoms are diagnosed.
Welsh health experts have just returned from a fact-finding visit.
Prof Olesen from University of Aarhus said part of the reason Wales was lagging behind many other countries was patients too often waited too long for a diagnosis.
As a result too many patients start treatment at a late stage when their cancer is well advanced or has become incurable.
In recent years Denmark has transformed the way its health service delivers cancer care, after international research suggested it was performing poorly compared to other developed countries.
Denmark's poor performance - it ranked alongside the UK nations in international league tables - was considered a "disaster" by Danish politicians and the medical profession.
One of the key changes introduced in Denmark was to develop a system where patients who are ill, but do not have clear symptoms of a specific cancer - can have diagnostic tests more quickly.
These can take place within a few days or even within a few hours of a GP making a referral.
Special "one stop shop" diagnostic centres have been set up at hospitals for those with more vague symptoms, while other open-access centres are able to provide quick one-off tests or scans and to report back quickly to GPs.
Similar patients in Wales can wait weeks or even months for those tests.
Prof Frede Olesen helped devise the new model of care in Denmark
Emerging research suggests Denmark is now closing the gap with the best performing countries on cancer survival.
"We can't say for sure yet whether it's the waits, better treatment, concentration of treatment or better equipment, but there have been calculations showing that waits really matter," said Prof Olesen.
"In my perception, there is no doubt shorter waits mean better prognosis."
A group of cancer specialists, GPs and health managers were shown the Danish model.
One expert said survival rates in Wales are "not as good as they should be".
Part of the problem is that patients with not obviously serious symptoms can get "lost in the system" - even though this group of patients ultimately account for around 50% of cancer cases.
Dr Tom Crosby, medical director of the Wales Cancer Network, said: "What they've demonstrated [in Denmark] is that what's taking us weeks and months in Wales to diagnose patients, particularly with those vague and non specific symptoms, they're now doing in a matter of days and there's nothing they're doing here that we can't do in Wales."
He said cancer patients in Wales generally had a very good experience in hospital but survival was not as good as it should be.
"This is more than just statistics, we know survival needs to improve but also it's devastating for us to see patients who complained of vague or non specific symptoms for months to be ultimately diagnosed with incurable disease."
But health bosses say they are confident that some of the changes introduced in Denmark can be replicated in Wales.
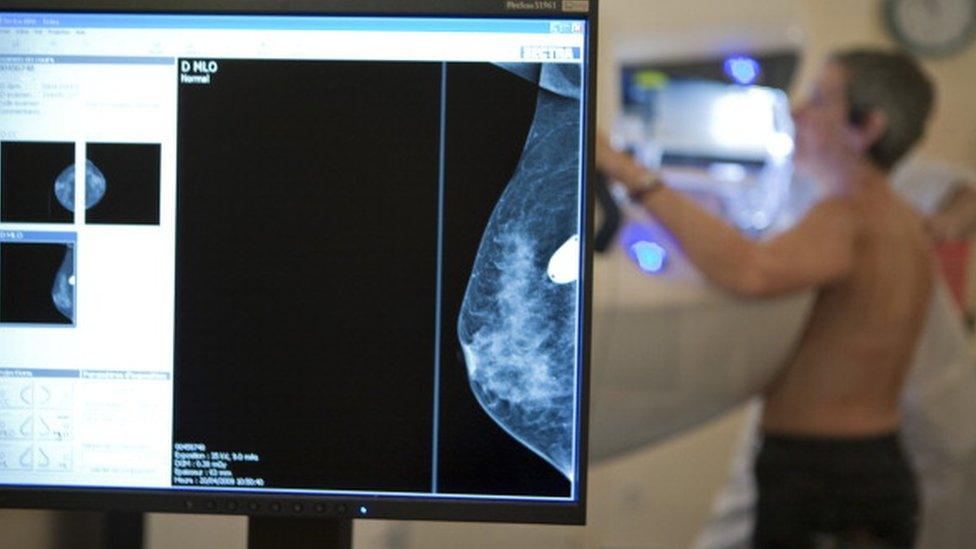
Nurse Glynis Watkins explains how her bad back turned out to be breast cancer
Cwm Taf Health Board in the south Wales valleys says it has already adopted some of the principles of the Danish model - for example in a project to diagnose head and neck cancers more quickly.
The health board is eager to hold further pilots, based on the changes made in Denmark, which, if successful, could perhaps be rolled out across Wales.
John Palmer, director of primary and community care at Cwm Taf, said they were already making progress in areas like breast cancer but they could "definitely scale up and do more".
"Every single day, NHS Wales does amazing things, mainly through collaboration - our multi disciplinary teams deal with highly complex work and most of the time deliver very effective services," he said.
"So I feel strongly we ought to be optimistic and there are real opportunities to roll out this work."
- Published11 April 2016

- Published1 March 2016

- Published17 February 2016

- Published11 March 2016

- Published16 March 2016
- Published4 February 2016
