Call to 'transform' cancer survival rates in Wales
- Published
Becky Thomas, a nurse from Merthyr, is now in remission from cancer but says patients must be listened to more
Three hundred more patients might survive cancer each year in Wales if services performed to the European average, a leading specialist has said.
That could be an estimated 600 lives saved if Wales ranked with the best.
Tom Crosby, medical director of the Wales Cancer Network, said there needed to be "a relentless drive to diagnose cancers earlier".
He wants the way services are delivered to be transformed or he fears they could "break" and "fall over".
Dr Crosby, consultant oncologist at Velindre Cancer Centre, Cardiff, said cancer services in Wales were already struggling to cope.
And with the number of people with the disease predicted to double by 2035 it could become more and more difficult to close the performance gap.
Although most patients in Wales have a good experience of cancer care - Dr Crosby said frontline staff go "the extra mile" - he believes step-by-step change will no longer be enough.
He wants lessons learned from countries like Denmark, where cancer experts from Wales have already undertaken a fact-finding visit.
"It shows what the prize is if we get this right and perform as other services do," said Dr Crosby.
"As a country, as health organisations, we have to accept that our outcomes are not as good as they need to be. We must all find that unacceptable and strive to improve those outcomes."

HOW IS WALES DOING?
Wales rates 21st out of 29 countries in Europe in five year survival rates for both prostate cancer and breast cancer.
An analysis of relative survival scores for bowel cancers across Europe ranked Wales well below average and one of the lowest - 23rd of 29 countries, behind Slovenia and Estonia.
With lung cancer survival, the same analysis of European countries ranked Wales 28th out of 29.

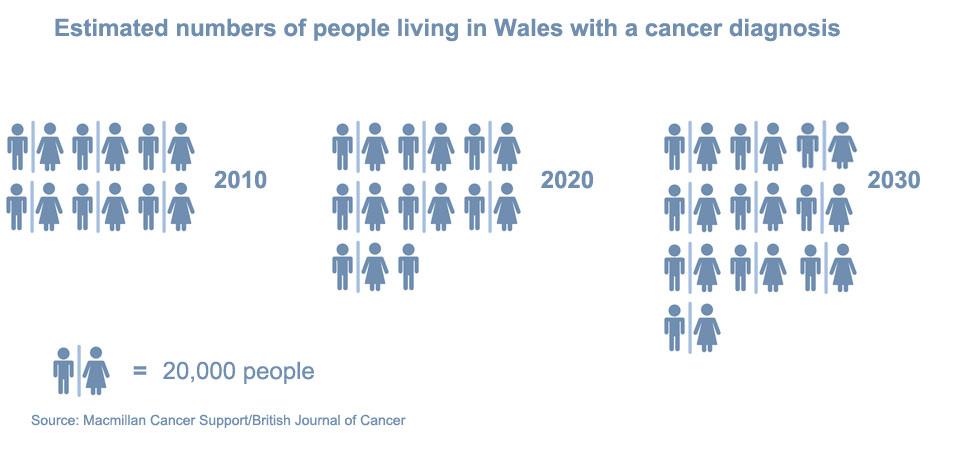
MORE PEOPLE LIVING WITH CANCER
It is estimated cancer cases will continue to increase by 2% a year, so a person born after 1960 would have a 50% chance of getting the disease in their lifetime.
But there is improved survival, with people currently living an average of about 10 years; unthinkable in the 1970s.
So, as well as more people being newly diagnosed with cancer, that also means the numbers of people living with cancer are estimated at doubling to about 220,000 in Wales by 2030.


Dr Cliff Jones says when symptoms are not clear cut, it can mean going "round and round" for a diagnosis
TRANSFORMING DIAGNOSIS
Cancer experts from Wales visited Denmark to look at how worrying survival rates were tackled - including with one-stop clinics which do a variety of tests at once.
Like in Wales, in Denmark if you have obvious or alarming symptoms these are almost always picked up. The challenge is how better to diagnose those patients with vague or harder-to-spot symptoms.
Pilots have recently started in the Cwm Taf and Abertawe Bro Morgannwg areas for GPs to refer patients with less obvious symptoms to diagnostic centres.
Joyce Thomas, from Pontardawe, was checked at a one-stop clinic in Neath
In Neath Port Talbot, all GP surgeries now have the option to refer patients to a "one-stop" clinic.
Since June, 13 patients have been referred and three of them were diagnosed with cancer.
Radiologist Sian Phillips said: "Patients have all their diagnostic investigations like blood tests, mostly CT scans and ultra-scans to put the jigsaw puzzle together to get as a rapid diagnosis as possible."
She said it has the potential to shorten the diagnosis process "by weeks, possibly months".
There is also a drive to train more radiologists while numbers of both experienced diagnostic clinicians and scanning equipment were lower in comparison to other countries.
Dr Crosby said diagnostic services such as radiology and pathology were facing "unprecedented demand" and "struggling to cope" but some suspect GPs might be wary of referring patients with less obvious signs for fear of overloading the system.
Susan Morris, head of services with Macmillan Cancer Support in Wales, said 93% of patients, in a recent survey, reported positive experiences of treatment but there were still issues over consistency and it was "not a time for treading water".
"We need to make sure we get the basics right. Not everyone gets written information about their cancer or their options and less than half were told about the future side-effects," she said.
"We need to make sure 100% of people get a clinical nurse specialist, get their wider care needs taken care of and no matter where you live, your experience is good."
WAITING TIMES
Cancer waiting times are fairly steady but Dr Crosby said there was still a long way to go and the health services "need to be doing in days, what is being doing in weeks".
He wants a combined and strategic approach with a change in the way GPs and hospitals work together.
Dr Crosby, who has made his case to the Welsh Government, wants an investment in regional diagnostic centres and has called for a cancer summit, inviting international experts.
Conservative health spokeswoman Angela Burns AM called for an independent review to develop a plan "to bring us into the 21st Century".
She added: "It cannot be right that countries from the former Eastern bloc rank ahead of us on so many indicators."
Plaid Cymru health spokesman Rhun ap Iorwerth AM said "excessively long waiting times for cancer diagnoses are a huge problem in Wales" and the party had "long set out" plans for three multidisciplinary diagnostic centres so patients with suspected cancer could receive a diagnosis or the 'all clear' within 28 days.
Andy Glyde of Cancer Research UK said: "To improve early diagnosis in Wales, the Welsh Government needs to ensure that our diagnostic services have the right workforce and equipment in place and that patients can move through the system quickly".
The Welsh Government said it was committed to delivering "the best possible care and support to everyone affected by cancer".
A spokesperson said more people with cancer were being treated within the target times despite an increased demand on services.
"Last year we saw a 40% increase in patients being treated within the 62-day target time compared to five years ago. But we know there's more to do to further improve services."
It is looking at improving early detection through changes in primary care, hospital referral pathways and regional diagnostic centres.
- Published5 July 2017

- Published22 February 2017

- Published20 April 2017

- Published12 April 2017

- Published20 July 2016
- Published11 April 2016

- Published20 January 2016
