Vaccination benefits need to be explained better, report says
- Published
Frank Atherton said older people needed to understand the benefits of getting the flu vaccine
Wales' chief medical officer has warned of the threat from anti-vaccination campaigners.
In his annual report, external, Dr Frank Atherton said people needed to be made aware of the benefits of vaccines.
In January, the Royal Society for Public Health said "misinformation" about the safety of vaccines was being spread on social media.
Unicef says more than half a million children in the UK were unvaccinated against measles from 2010 to 2017.
The chief medical officer's report says the rate of two year olds in Wales getting the first dose of the measles, mumps and rubella (MMR) vaccine is below 95%.
That is the rate required to protect a population from a disease, according to the World Health Organisation.
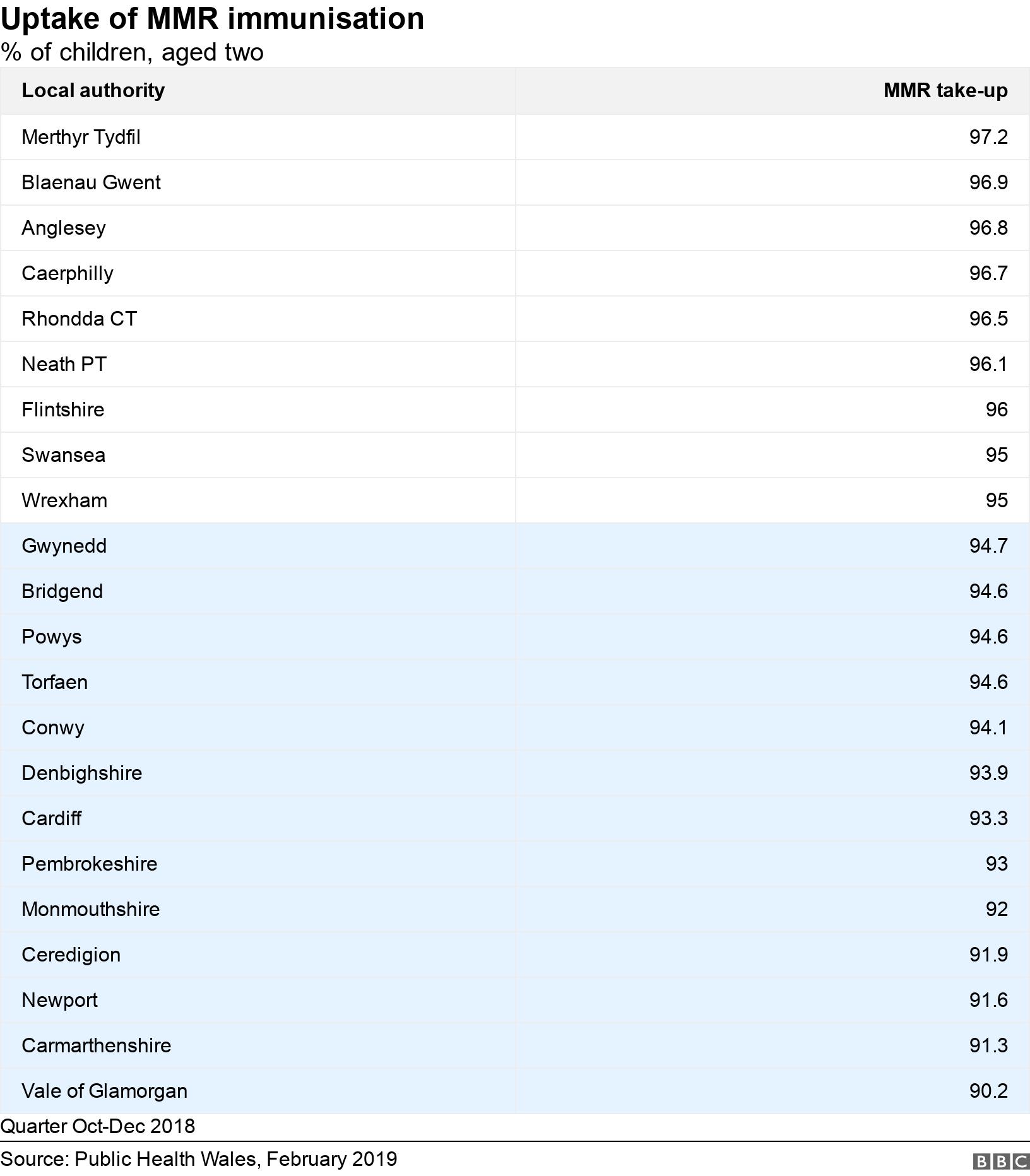
Latest figures show 94.3% of two year olds received the MMR vaccine in Wales - but more than half of local authority areas were below the 95% target.
The lowest proportion was just over 90% in Vale of Glamorgan, but the immunisation programme was doing better on Anglesey and in the south Wales valleys, traditionally more deprived parts of the country.
The highest take-up was in Merthyr Tydfil, with 97.2% of two year olds getting the jab.
"Most people do choose to be vaccinated, but a small minority remain unconvinced by the safety and benefits of vaccines," Dr Atherton said.
"We need to work with clinicians and other experts to ensure that parents are fully informed of the benefits of vaccination, to ensure maximum uptake of the vaccine and achieve our aim of eradicating preventable diseases.
"Similarly older people need to understand the health benefits to them of vaccination against influenza, pneumococcal disease and shingles."

What is measles?
A highly infectious virus spread in droplets from coughs, sneezes or direct contact
It can hang in the air or remain on surfaces for hours
It often starts with fever, feeling unwell, sore eyes and a cough followed by a rising fever and rash
At its mildest, it makes children feel very miserable, with recovery in seven to 10 days - but complications, including ear infections, seizures, diarrhoea, pneumonia and brain inflammation, are common
It is more severe in the very young, in adults and in people with immunity problems
Still a major cause of child death in many low-income countries, although the measles vaccine is thought to have prevented more than 20 million deaths in 2000-17


Measles is still a major cause of child death in many low-income countries
Students were urged to make sure their vaccinations were up to date following reports of cases of mumps at Cardiff Metropolitan University in April.
Last year, Public Health Wales asked parents to get their children vaccinated after outbreaks of measles around south east Wales.
Sonia Davies, a retired nurse and health visitor from Llanelli, told BBC Radio Wales people have become "complacent" about vaccines.
"I would give them all the information I had available, but at the end of the day it is their choice," she said.
"It can be very frustrating indeed, it's not an argument, we are giving them the facts and the facts speak for themselves and all you do is encourage them to reconsider their views.
"People have become very complacent about childhood diseases, they don't realise how serious they can be."
Speaking to BBC Radio Cymru, Dr Phil White, who leads on vaccines on the British Medical Association's GP committee in Wales, said people who spread misinformation should face action.
He said: "They're doing this on purpose. There is no scientific evidence whatsoever to what people are saying, and maybe they should be taken to court... It's the only way.
"We've seen this on the internet - it's quite a problem - a lot of untruths are being told and somebody needs to do something about it."
The report also looks at the threat from resistance to antibiotics.
Global overuse of antibiotics has led to a reduction in their effectiveness, as bacteria grow immune to them.
The report says this has already led to a small number of difficult to treat infections, leading to "failed therapy and potential complications".
A focus on reducing antibiotic use in GPs' surgeries saw a fall of nearly 12% in their use over five years, the report added.
- Published27 January 2019

- Published24 April 2019

- Published28 March 2018

- Published29 April 2019
