Coronavirus: Royal Glamorgan Hospital staff on life on front line
- Published
Inside intensive care: "Your loved ones are not alone"
"Be a home hero for us." That is the stay-home message ahead of the Easter weekend from staff fighting to save lives inside the Royal Glamorgan Hospital.
Two friends and colleagues on the coronavirus front line - a consultant anaesthetist and a consultant in intensive care - told BBC Wales of the challenges of their work.
But they spoke also of missing their extended families and hugs from their children - and the pressures staff are under in this unprecedented time in their medical careers.
The Royal Glamorgan had this afternoon one spare intensive care bed - and they are starting to see a surge.
Currently, Cwm Taf Morgannwg health board says it has 36 patients being cared for in intensive care and associated ventilated beds.
There are also 112 patients with Covid-19 being cared for on wards.

Friends and colleagues - Ceri Lynch and Nerys Conway outside the hospital
How busy is it?
Ceri Lynch, consultant anaesthetist
"It's very busy. By definition anybody who's in intensive care is critically ill and is sick enough that they may not survive. We're full at the moment. And we've made plans to expand our capacity to three times or even four times our usual."
Nerys Conway, intensive care consultant
"Numbers have really increased in admissions in the last week. There's been a marked difference and we certainly have seen a surge of patients that have been coming in with Covid-19."

Nerys Conway, consultant in intensive care
What are you seeing?
Nerys: "It's not appropriate for everyone to go to into intensive care. Some patients can be managed at home, in the community. Others will need just a little bit of oxygen on the wards, with some intravenous antibiotics, but others unfortunately will need that care that Ceri and her team will provide."
Ceri: "Some are older, some are younger. Some have got other health problems and some have been previously fit and well before they caught Covid-19. In other ways they're all very similar. They're all presenting the same problems - trouble breathing, needing extra oxygen, needing help with their breathing, and all of the ones in intensive care are on a ventilator to help with their breathing.
"Some are very sick, some have died, some will die.
"We were led to believe from the information from China and Italy was that it was preferentially affecting older people with existing health problems. That's not what we've been seeing in Wales.
"We've been seeing young, fit and healthy people critically ill with Covid-19."
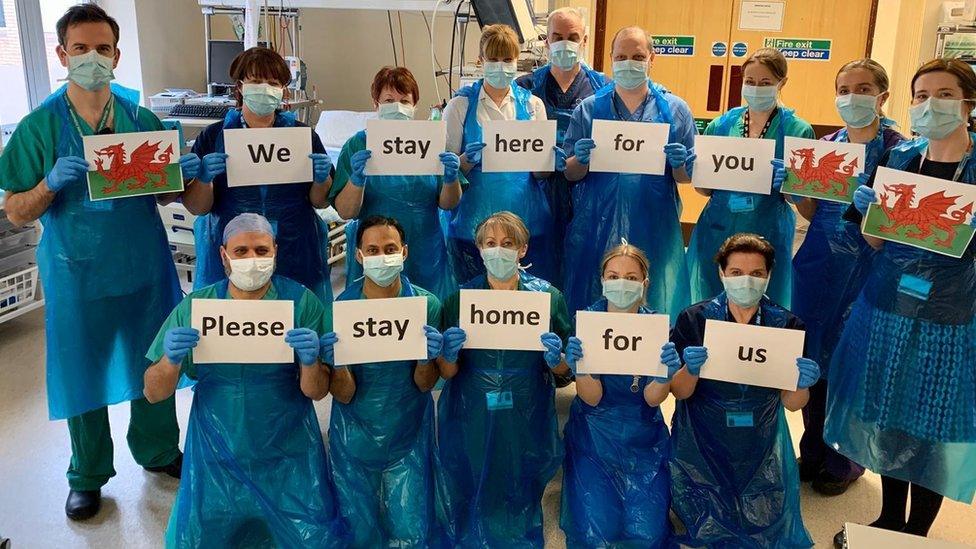
The message is clear from staff at the Royal Glamorgan
How does this impact on you and other staff?
Nerys: "Some patients have very minimal symptoms and others are incredibly unwell and need critical care, and there is that worry, but also as well the psychological impact that it has on us.
"What we're seeing - and the conversations that we're having with family over the phone - that does create a level of anxiety.
"There are people that are my age coming into our A&E department who are fit and well, they never see their GP, they have no medical problems and they're not on any medication, and they're coming in very unwell with Covid-19 and going into intensive care."

Ceri Lynch, consultant anaesthetist
Ceri: "We've had amazing work by the whole hospital, all the staff have worked together really well. The engineers have been working around the clock to make sure we've got enough oxygen for example, it's been fantastic.
"But it's exhausting, actually you feel very hot all the time using personal protective equipment (PPE). Everything is more challenging because you can't see or hear properly."
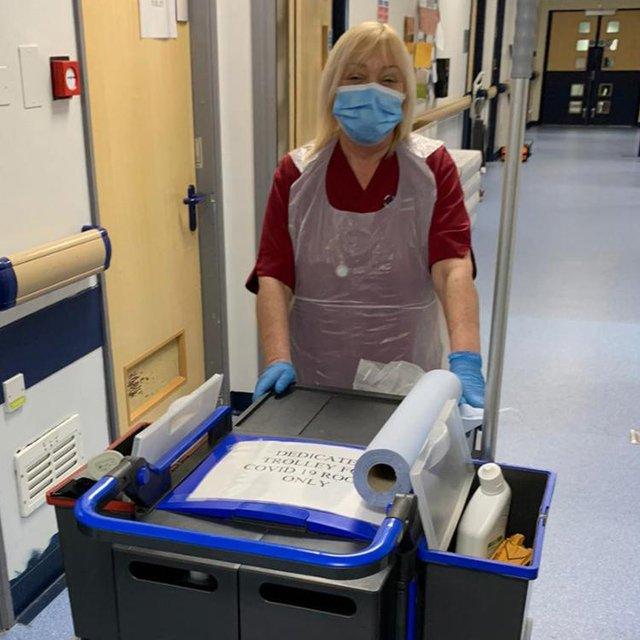
Staff are given rests very few hours so they get a break from protective equipment

"Communication is very difficult because you can't see people's faces and everything has that added layer of difficulty getting in and out of the PPE.
"It adds time delays and people are finding that tiring and a bit overwhelming at times and we're having to support each other.
Nerys: "We are reviewing the PPE situation every day. We have a dedicated team for PPE and are in daily conversation with Welsh Government with regard to PPE and ventilators, so I do feel safe at work."

How about dealing with death?
Ceri: "We encounter death quite frequently in intensive care anyway. What's different is that we don't have the families present all the time, like we usually do. Having these conversations over the telephone is much more challenging for both sides.
"It's very sad, but I want the families to be reassured their loved ones are not on their own. We are with them, they have a one-to-one nursing staff with every patient, and they are holding their hands. They are talking to the patients, they're speaking to the families every day and finding out information about the patient, so we get to know those patients."

Staff send a message about staying at home

What about your own families?
Nerys: "It's really tough. It's been really hard and very challenging for everyone. I'm really missing my parents, my in-laws, my sister, her family, my extended family, my friends. It's there, my support network - my husband and my son are just absolutely keeping me going, they've both been absolutely fantastic.
"I'm just taking the necessary precautions and making sure that I shower before I leave. Making sure that I'm using the equipment correctly and at home we're hand washing and meticulous about the cleaning."
Ceri: "I'm doing the job that I love. I'm tired because everyone's working longer hours. We're doing long days and night shifts. It's hard because I'm not seeing my parents, my brother and sister and extended family who were further away.
"And my husband and children are worried about me going to work every day, worried about me catching the virus, and I'm trying to distance myself from them in the house, so I'm not having hugs with my sons, which is very difficult, it's really hard for me and them."
How do you see it developing?
Nerys: "It's difficult to know when normal will resume - and of course how wonderful normal was."
Ceri: "I think we'll have more and more patients coming through.
"Patients don't just stay for a few days and get better - they're all with us for at least 10 days, maybe two weeks. And then it's going to take them months - the survivors - it will take them months to get back to normal. If they ever do.
"So this is going to be a problem for a long long time."

Nerys Conway and colleagues in full protective gear
What's your message to the public?
Ceri: "Stay at home and stay safe. Please don't go out over the Easter holidays, please don't catch the virus or spread the virus."
Nerys: "I think that everyone at home can help us. People can be a hero and be part of this with us. So be a home hero for us. Be part of this with us, help us help you."
- Published7 April 2020

- Published6 April 2020

- Published4 May 2020
