Coronavirus: 'Huge deficit' in critical care doctor training
- Published
- comments
"Huge deficit" in intensive care doctors
More intensive care doctors need to be trained in Wales to address a "huge deficit", a senior medic has warned.
Jack Parry-Jones said most of Wales' intensive care units were short of doctors before the coronavirus pandemic struck.
He called for more training places for intensive care doctors and for the units themselves to be upgraded.
The NHS body responsible for training said there had been a "sustainable increase" in training places.
A Welsh Government spokesman said: "We are committed to improving critical care capacity across Wales.
"The health minister set out a programme for improving critical care, including £15m of funding. We have also featured critical care as part of our Train Work Live, external campaign."
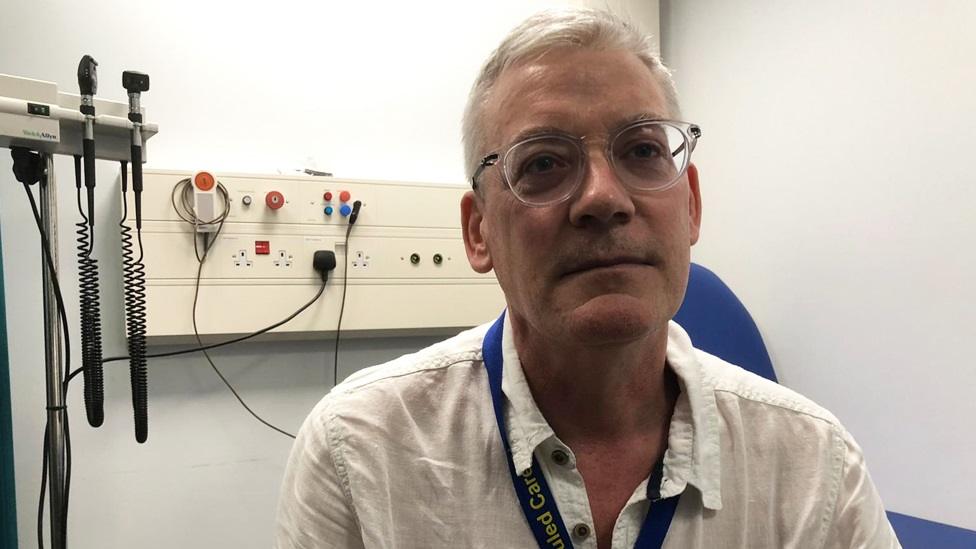
Jack Parry-Jones said other health boards needed the same investment in critical care units as the Aneurin Bevan board was making at the new Grange University Hospital
Dr Parry-Jones, who is an intensive care consultant in south Wales and a board member of the Faculty of Intensive Care Medicine, said units were staffed by doctors who were not necessarily specialists in intensive care medicine.
"Most units are short of intensive care medicine doctors, and that would be from consultants all the way through to juniors.
"But the important thing really is that 50% of intensive care posts are not properly filled. And by that I mean that most intensive care units in Wales still require the intensive care consultant rota to be covered at some point by people who aren't intensive care medicine trained."
He said they tended to be anaesthetic consultants who "cross-covered" into intensive care, as opposed to fully-trained intensive medicine consultants.
The organisation responsible for training doctors, Health Education and Improvement Wales (HEIW), said there had been a "planned, sustainable increase" in training places in recent years.
Pushpinder Mangat, HEIW medical director and a former intensive care consultant, said: "Since 2017 we have increased the number of permanent higher speciality intensive care training posts in Wales by 58%.
"We have continued this plan with new posts for this year's intake and plan to include further posts next year."
He said they had also increased the number of internal medicine training posts, meaning every year an extra 39 trainee doctors would work and gain experience in Welsh intensive care units.
But Dr Parry-Jones said while the number of trainees had increased there was still a significant shortfall.
"There's a huge deficit because we have a deficit anyway, and then obviously we have consultants retiring all the time. And there's a constant fill-rate that needs to go on just to maintain the status quo."
He said there would eventually be "limits" to how many trainees could be taken on, but that was not the case at the moment.
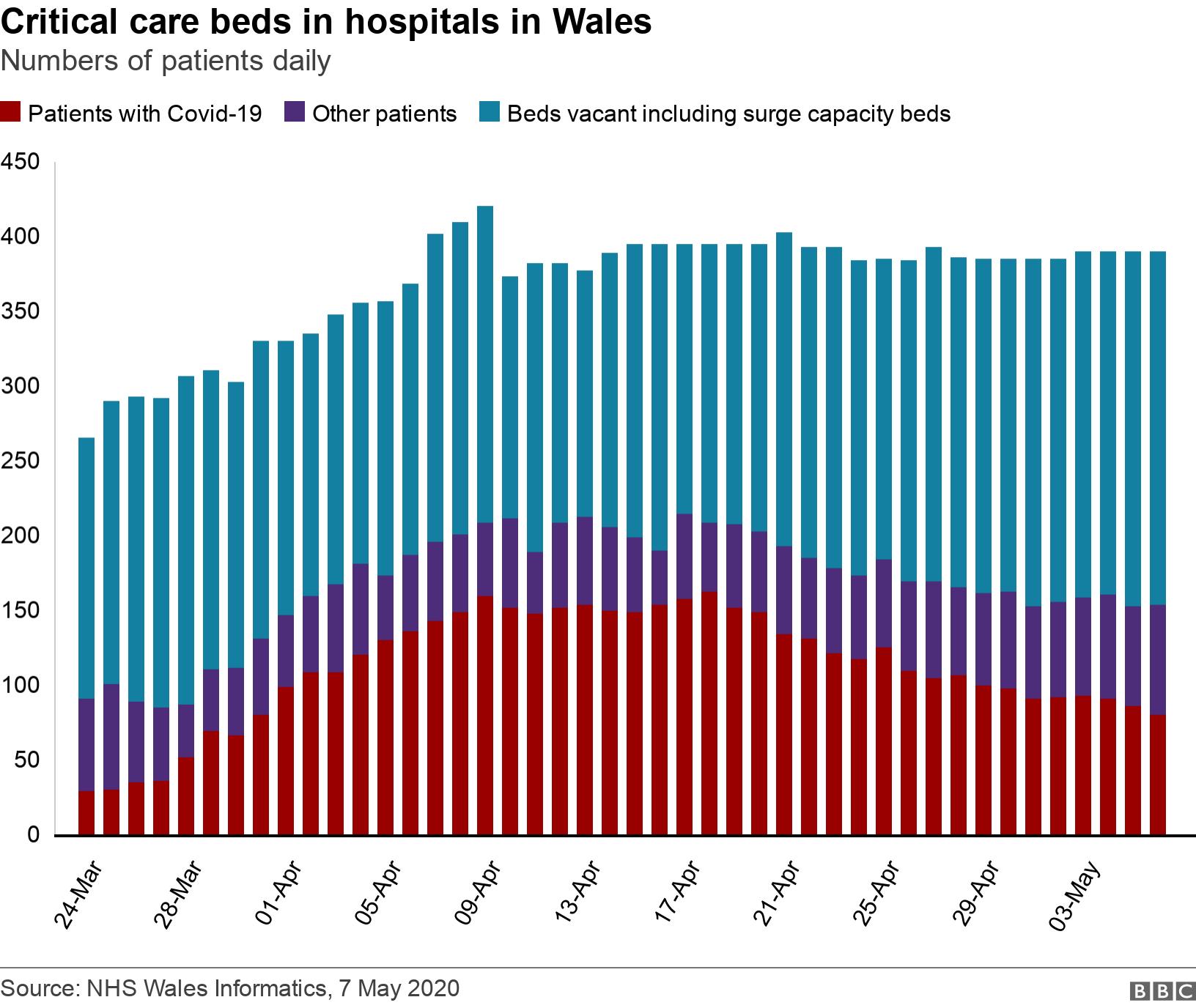
During the coronavirus pandemic, extra "surge capacity" beds have been made available in hospitals to cope with the potential numbers of critically ill patients, on a temporary basis.
Conservative health spokeswoman in the Senedd Angela Burns said shortfalls across the NHS needed to be addressed for it to cope with the pressures it faces.
Ms Burns said: "With sadness I think this pandemic is not going to be the only time we are under this kind of pressure. So we have to absolutely make sure we can ramp up the resources we need."
She said expanding capacity to cope with the pressure meant the right staff needed to be recruited.
"These people take an awfully long time to train because they are highly specialised. Getting the bed is one thing, getting the right calibre of people to staff it is completely different."
Dr Parry-Jones said the units themselves needed upgrading to match the standard that would open at the new Grange University Hospital near Cwmbran next year, which will have 30 intensive care beds, all of them isolated.
"We've been trying to do the increase [in training posts] for many, many years. For 10 to 15 years we've been asking for an increase. I think the Welsh Government really picked up and started listening to this about two years ago now."
He said Cardiff had far too few isolation facilities and that investment was needed "to bring it into the 21st Century."
- Published11 May 2020

- Published11 March 2020

- Published24 April 2020
