Covid: How have doctors coped with pandemic frontline?
- Published
Doctors talk about their experiences working during the coronavirus pandemic
The coronavirus pandemic has been testing for all of us, but what about those who have spent a year on the healthcare frontline?
On the anniversary of Wales' first lockdown, three doctors share their experiences of the past year and the impact the coronavirus pandemic has had on them.
'I was inspired by brave and courageous colleagues'

Faris Hussain said this year has "cemented" his commitment to medicine
As a junior doctor, Faris Hussain, 25, from Caldicot, is doing what is known as his "F1", or first foundation year.
He is three months into a four-month placement on the intensive care unit at the University Hospital of Wales in Cardiff.
"There was a period of about five, six weeks, where it just felt non-stop and absolutely knackering from the point of view of the doctors," he remembers.
"I've been asked how my night shift has been when in fact I've only just turned up to start my day shift", Faris said, adding that at times work has been "exhausting".
"I think most of the staff members I've spoken to have felt that this is one of the longest winters they've ever worked.'
However, Faris said this year has "cemented" his commitment to medicine.
"I find that what has mostly inspired me has been the work of my colleagues.
"We saw a lot of sad cases of quite young people not doing terribly well in intensive care. But I found that despite all that, a lot of the healthcare professionals were very brave and courageous in that they were still able to do sort of everything they can, to make patients comfortable or just looking after the sheer number of patients that were coming to us with Covid and I've found that really inspiring."
'The hardest times were breaking bad news'

Eli said the hardest times have been breaking bac news to families who could not be with their loved ones
Eli Wyatt, 24, from Monmouthshire is also a junior doctor doing her "F1".
She's currently working on a renal ward at the Glan Clwyd Hospital in Denbighshire and believes she is starting to see the "other side of Covid".
'Recently we seem to be getting a lot of patients with quite extensive cancers, who have been diagnosed quite late on, and I wonder whether this is the kind of side of Covid that we're maybe not seeing," she says.
"As a sort of side effect to the pandemic these people have probably been shielding for a while, might not be going to the GP quite as often as they should, or would have been prior to the pandemic. And it means that these cancers are being picked up quite late on."
As part of the "F1", junior doctors do rotations in different departments at hospitals and Eli has previously worked on Covid wards
She said that despite feeling "scared" about the risks to her own health, she felt it was her "calling" to help out.
"I think the hardest times were when I was breaking bad news over the phone to patients' families and not being able to have that conversation in person, I really struggled," she says.
"Because I think it takes away from what we've been trained to do and what we've had experience of doing and I do feel for the patients and families who've had to have bad news over the phone and not in person."
'They're not just a name, they're somebody you know'
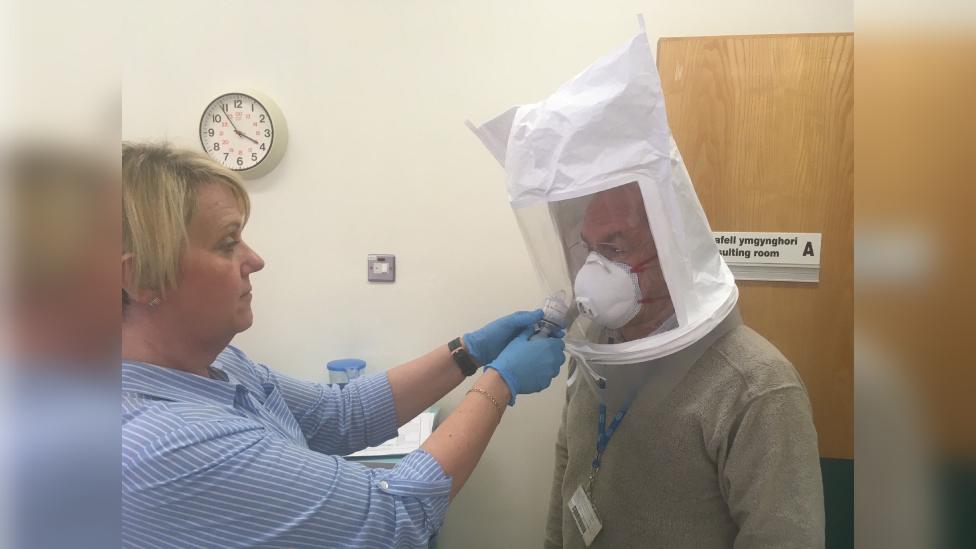
Peter said the risks of his age and Covid was not going to stop him working on the frontline
Dr Peter Saul is a GP, from Wrexham, who has worked as a doctor for nearly 40 years and is the joint chair for the Royal College of GPs in Wales.
He said: "Putting an arm on somebody's shoulder when you're reassuring them after difficult news. It can be very powerful and we've not been able to do that, to get physically as close to people to reassure them as we would have liked.
"The autumn and winter to me seemed worse than the springtime. Things were ramping up, we were having to learn new ways of working, I was doing more out of hour shifts to cover that.
"In my practice we've got a notice board where we put on the patients who have passed away and it was just filling up, day after day, and as a GP these are people you know, they're not just a name, they're somebody that you know, you know their families and it takes its toll on the clinicians, and it takes its toll of the administrative staff."
Peter, who is aged in his 60s, said he agreed that helping the NHS during the pandemic felt like his "calling".
"People said to me, you know you're at higher risk you don't need to do this, but I actually felt I needed to do it. I've been a doctor all my life, I wasn't going to stop being a doctor."
More on Wales Live 22:35 GMT, BBC One Wales.
- Published22 March 2021

- Published22 March 2021

- Published22 March 2021
