Infected blood inquiry: Diagnosed with HIV at 15 then 'left to go and die'
- Published
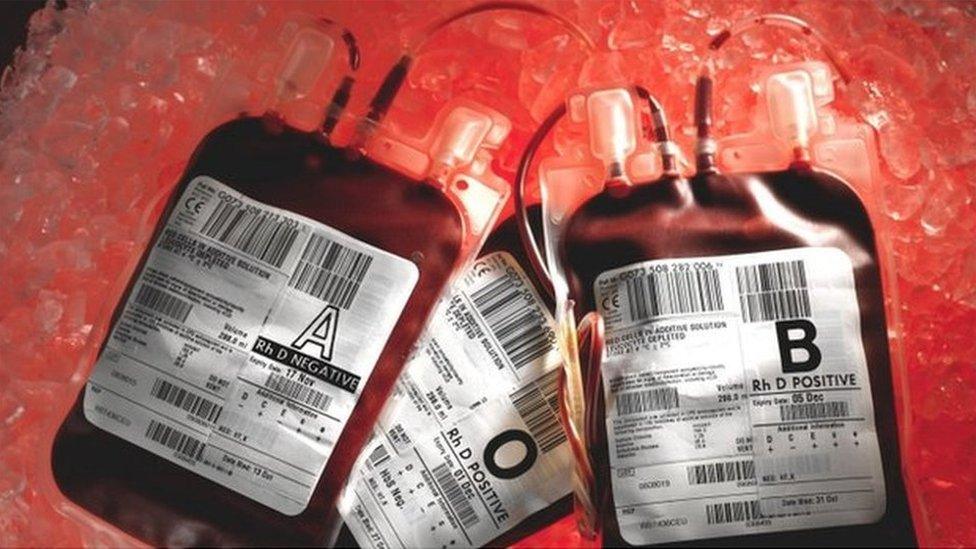
Up to 30,000 people were given contaminated blood in the UK, and thousands died
A man infected with HIV and hepatitis C through blood products in the 1980s has told of his shock diagnosis as a teen.
Speaking anonymously to the Infected Blood Inquiry, he said he and others at a school for disabled children were "left to go and die".
More than 120 haemophiliac pupils were given infected blood at Treloar's College, Hampshire.
His south Wales valleys upbringing made it hard to talk to his parents about his condition, he said.
The infection of up to 30,000 people with contaminated blood, which killed thousands, has been called the biggest treatment disaster in NHS history.
The public inquiry has been taking evidence since 2019 from people affected by the scandal.
The witness, who received treatment for his haemophilia, a blood condition which affects the clotting of blood, at the college, said he was about 15 when he was given the diagnosis.
At the time, he believed he would only have two to three years to live.
Now a grown man, he told the inquiry he felt the government may not have acted in the same way in the 1980s if the general population had been more widely affected than minority groups such as haemophiliacs and gay men.
He said there was no support for him, despite being infected as a child through a catastrophic error.
"I think I was in too much shock, but I can't remember being offered any form of counselling," he said.
"There was never a counsellor and nothing like that was ever spoken about and of course you're giving effectively a terminal diagnosis to a teenager."
When asked what his understanding of the diagnosis was in 1985, the man said: "I was going to be dead within two to three years".
He was diagnosed with haemophilia aged three when he broke his leg, the inquiry heard.
In 1975, at the age of six, he said he received experimental treatment for the condition which left him unable to go to school for more than a few days a year, suffering from bleeds which would last between 10 and 14 days.

Treloar's College, where more than 120 pupils were infected with HIV and hepatitis
He described being sent to Treloar's school for disabled children as "transformational", as it meant he was able to interact with other children of a similar age.
But it was here that his life was turned upside down.
'Left to go and die'
He told the inquiry the stigma meant that he had been unable to talk meaningfully about his diagnosis with his parents.
"If I'd said 'dad I've got cancer', or something like that, we'd have had a conversation about it.
"We'd had conversations about haemophilia and how it was going to affect you but no, you couldn't talk about it. And part of that was growing up in a Welsh valleys mountain town where everybody knew everybody else's business."
The inquiry heard that the way HIV and Aids were viewed at the time added to his feelings of isolation.
"In 1985 you were told you were probably going to die in two years and in some senses the government set up an environment that ostracised us and basically made us scared and made the general population scared.
"So rather than receiving any kind of support and help or anything like that we were effectively left to go and die with our families in houses behind locked doors."
'They should have protected us'
He told the inquiry that he has had difficulties with personal relationships at different times in his life and has suffered from poor mental health.
He also found employment difficult and felt a degree of "survivor's guilt".
"Why was I the lucky one who survived when I could name 20 names that didn't? That doesn't wash.
"The diagnosis of HIV, the unfairness of it. In some sense anger at the way we were treated in the '80s. The ostracisation of us. That really wasn't fair and very inhumane and all of these issues started to come with a sense of worthlessness.
He said the government at the time should have been more proactive.
"They should have protected us more than they did," he said.
"If the general population were affected, would their actions have been the same? I honestly don't know."
- Published2 February 2021

- Published24 February 2021

- Published21 June 2021

