HPV & Cervical cancer: New screenings will save lives - top doctor
- Published
A top doctor has defended changes to cervical cancer screening, saying they will "help save lives"
Changes in cervical cancer screenings will help save lives, not put them at risk, according to a top gynaecologist.
Prof Alison Fiander said people should not be worried screenings have dropped from every three to every five years in Wales as tests are "more effective".
Public Health Wales (PHW) said the new rules were for people aged 25 to 49.
Rachel Paul, whose UK-wide petition attracted 1.2 million signatures, believes the decision is "playing with people's lives".
Two Labour Members of the Senedd challenged their own government in a debate on Wednesday after 30,000 signed a Senedd, external petition calling for change.
Women and people with a cervix - as it could also affect transgender men - who have not tested positive for human papillomavirus (HPV), external will now wait two more years between tests.
Health chiefs in Wales said they changed the interval between screenings to the same time as those in Scotland because tests are now more accurate. Cervical screening gaps in England and Northern Ireland remain at three years.
But Wales' public health body did publicly apologise for causing "concern", and admitted health chiefs "hadn't done enough to explain the changes".
Prof Fiander, a clinical lead at the Royal College of Obstetricians and Gynaecologists, said PHW had "missed an opportunity" to help educate people but reassured the public the change was safe and not a cost-cutting exercise.
She was involved in the HPV vaccine rollout in Wales, which data shows can cut cervical cancer by 90%, and says having the jab and screening together "can actually beat cervical cancer completely".
What has the reaction been?

"I started the petition to give people a voice," says Rachel Paul
Rachel Paul, 29, from Llanelli, wants those who have missed an opportunity to have a HPV vaccine to still be offered the chance to have three-yearly appointments.
"My concern was - regardless of the science - people at three years don't always attend. Maybe they've delayed it by two years, that'll be five years already," she said.
"There could be people not attending smears for seven years because of self-consciousness."
Ms Paul said she has received between 30 and 40 messages since launching the petition from women "saying I am that 1% of the population who slipped through the net".

Catherine Jones says she was "surprised" to find out about the changes online
Catherine Jones, from Wrexham, said the PHW apology helped her understand the reasons behind the change but "I don't think they've put enough out there to explain it very well".
"Just an apology… but what have they actually done? All I've seen is what's in the media."
She said leaflets in GPs, social media campaigns and longer appointments explaining the screening process could bring clarity to worried women.
"If they're saying people under 30 are snubbing smearing, maybe they should focus on campaigning people to go for smears and educate."

Maria Dullaghan says she is not convinced these changes are for the best for the age bracket
Maria Dullaghan, who started cervical cancer therapy on her 26th birthday and needed a hysterectomy, is still not convinced about the changes.
"The age range they're looking at changing, the 25 to 49-year-olds, mostly haven't had the vaccine yet," the 37-year-old from Haverfordwest in Pembrokeshire told BBC Radio Wales.
"Maybe about three-quarters of my friends that age haven't had it yet - so I don't think it's a good idea.
"I had a clear test and then had my diagnosis within five years of that, so I don't want to see people going through what I did.
"The changes also haven't been communicated clearly, I think people feel a bit caught out by it coming in quietly at the start of the year."
During Wednesday's Senedd debate, Buffy Williams, MS for Rhondda, said she was among the women who feel aggrieved at the changes.
"Women should have the right to decide when they'd like to attend a screening appointment - be it three years or five years, or anywhere in between, regardless of the improved test."
She, like Ms Paul, feared five-year intervals could become more like ten for some women.

Buffy Williams said day-to-day life can get in the way of women attending appointments
Jack Sargeant, Alyn and Deeside MS and chairman of the petitions committee, said such an important decision "should have been carefully and fully explained", and social media "should not have been used for a way to announce such an important issue".
He called for PHW to reflect and review their policies for the future, but added: "I was also disappointed that such a significant change in our public health approach was not announced by the health and social services minister on the floor of our parliament in advance of the changes".
Health Minister Eluned Morgan said HPV caused changes to cells slowly over several years, and testing more frequently than five years could give an "incorrect reassurance".
Extending the screening intervals for low risk individuals means it can focus on those at high risk, she said.
She said the change had not been made to save resources, or because of the success of the HPV vaccine.
She said PHW had communicated it in a "calamitous way".
Dr Sharon Hillier, director of the Screening Division for PHW, provided reassurance that the change "is safe" and that the decision-making is based on recommendations from the UK National Screening Committee.
Why is cervical screening important?
Screening is not a test for cancer, but sometimes the test does pick up early cancers.
What happens during a smear test?
Cell changes found through regular cervical screening can be treated to prevent a cancer developing. Cervical cancers, external found early are easier to treat.
"What's important is that people attend screening when they're invited to do so," said Ms Fiander, a former gynaecological cancer surgeon at Cardiff's University Hospital of Wales.
"Because they will be tested for HPV and if they're negative they're not at risk of developing cervical cancer."
How dangerous is cervical cancer?
Cervical cancer is the most common cancer in women under the age of 35 in Wales, with about 160 people diagnosed every year, and is the 14th most common cancer in UK women.
A mum tells how a routine smear test led to her receiving life-saving treatment
Across the UK, there are about 3,200 new cases every year, with about six in 10 people diagnosed living a further five years, according to Cancer Research UK data.
There are around 850 cervical cancer deaths in the UK every year and the charity said relative five-year survival rates are below the European average in England, Wales and Scotland.
Around the world, cervical cancer is the fourth most common cancer in women, killing more than 300,000 each year.
What are the screening changes being made in Wales?
The new process means women and people with a cervix who had not tested positive for HPV, external will now wait five years instead of three between tests.
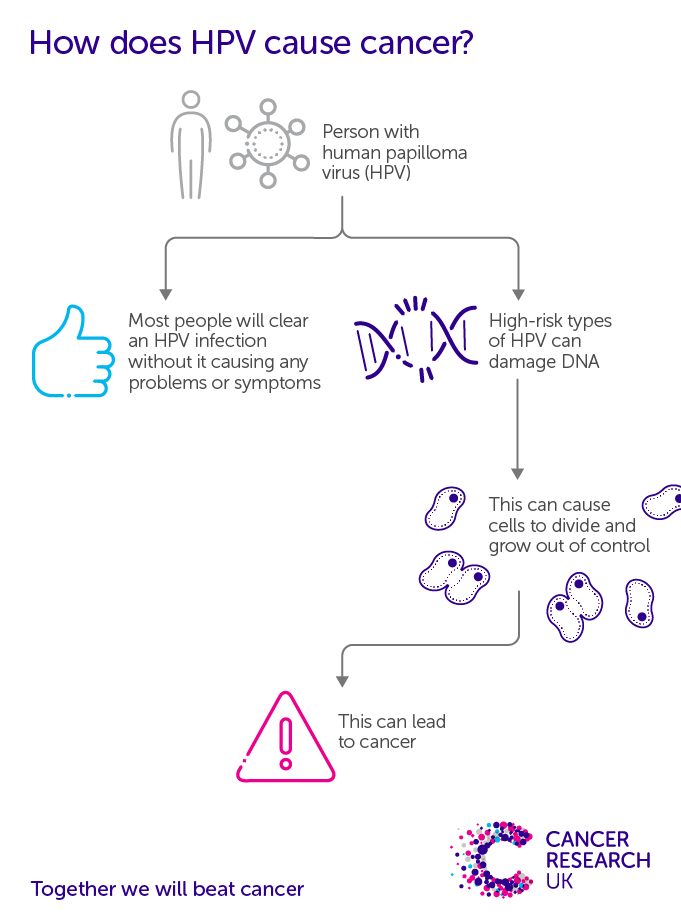
Cancer Research UK have done a lot of promotion explaining the new changes

"It's based on the science that over 99% of cervical cancers are caused by HPV," added Prof Fiander, a women's health masters course lecturer for online platform Learna.
"The cervical screening programme is using a new test, testing for HPV and that's more sensitive than the old method of screening, which was looking for cell changes from the cervix. It allows us to pick up women who are at risk of developing cervical cancer earlier than before.
"For people who have already tested positive for HPV or have been seen in colposcopy, external, which is where we see women with an abnormal smear, they will be followed up more closely.
"In terms of the experience of being screened, it's exactly the same for HPV screening.
"A smear is taken from the neck of the womb, the cervix, so the process is exactly the same it's just that it's tested in a different manner."
HPV is a very common virus that most people will come into contact with at some time during their lives but PHW says one or more high-risk type of HPV is present in more than 99.8% of cervical cancers.
Why are the cervical cancer screening changes being made?
PHW said the changes are evidence based - and follow a recommendation from the UK National Screening Committee in 2019, bringing the advice for this age group in line with the screening interval for those aged between 50 and 64.

We are all used to doing home tests after the Covid pandemic, but Dr Fiander says we could soon see this for HPV tests
"If you haven't got HPV, you're not going to develop cervical cancer," added Prof Fiander.
"Even if you get a HPV infection the day after screening, it takes between 10 to 15 years for cervical cancer to develop so leaving the screening interval for five years is absolutely fine as long as you go and get screened when you're invited.
"In the majority of cases, the HPV infection will be cleared by the immune defence system in two to three years without any intervention - and you don't want to undertake unnecessary treatments. That's the sort of science that's underlying the changes."
HPV testing was successfully introduced in Wales in 2018 and PHW said almost nine out of 10 results show no high-risk HPV.
"It's true that HPV vaccination is already decreasing the number of women that are developing pre-cancerous changes," added Prof Fiander.
"So I think combining HPV vaccination with cervical screening means that we could possibly eradicate cervical cancer in the UK, within a few generations which is really exciting.
Why are girls from ethnic minority backgrounds less likely to have the HPV vaccine?
"But it does mean that everybody that has a cervix needs to be vaccinated and, until then we do need to carry on with screening."
In the UK, girls are offered the vaccine between the ages of 11 and 13, depending on where they live. The vaccine has also been offered to boys since 2019.

HAYLEY PEARCE PODCAST : Tackling the issues that make your group chats go off
COMING OUT: From secrets to social media, conversations from the LGBTQ+ community in Wales

- Published10 January 2022

- Published6 January 2022

- Published5 January 2022

- Published4 January 2022

- Published4 November 2021

- Published13 September 2021

- Published12 March 2019
