Mental health: Patient's love-hate relationship with medication
- Published
Chronic illness medication 'emotionally challenging'
"When I look in the mirror I don't see me, I don't see the person that I used to be."
Helen Presdee-Jones says she has a "love-hate relationship" with the steroids that changed her appearance but are keeping her alive.
She emphasised the need for emotional and wellbeing support for those living with long term, chronic illnesses.
The Welsh government said it has raised funding to "improve access to a wider range of psychological therapies".

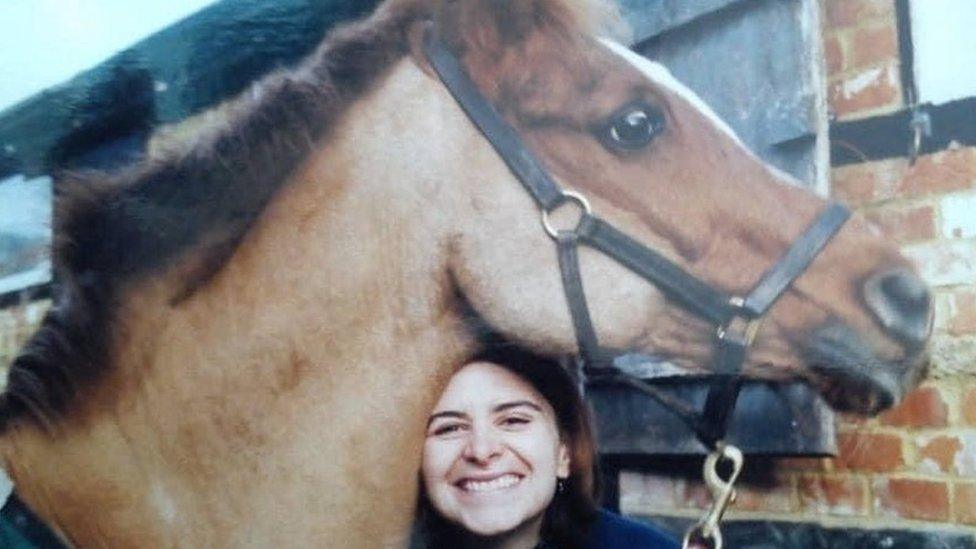
Helen Presdee-Jones feels that the steroids she takes following a kidney transplant give her a 'moon face'
Helen, 43, who lives near Cross Hands in Carmarthenshire, went into renal failure at 16 and has since had two kidney transplants.
Complications mean she must take steroids for life, giving her what she described as a "moon face" and prompting weight gain.
"I don't want to be in photographs now," she said.
"There's definitely a love-hate relationship," she said. "If I don't take them I will lose my transplant, but if I do take them, I have to deal with these other side effects."
Helen has also successfully been treated for a benign brain tumour and cervical cancer in the past four years.

Helen before she began taking medication for a kidney transplant
She reached a point last year where she needed therapy to help process her feelings.
"All of those emotions built up, and because of my cancer treatment I went into early menopause - that was a big milestone," she said, "because it meant the option of having children was a closed door."
She is now a supporter of the charity Daring to Dream, external, which focuses on the emotional wellbeing of adults in Wales with chronic illnesses.

The charity Daring to Dream is creating quiet rooms in hospitals
One of the charity's initiatives transforms hospital rooms so they can be used as quiet spaces for patients to be with loved ones, or to have private conversations with clinical teams.
"When it comes to the NHS, space is a premium," Helen said. "I was told I had a brain tumour in a hospital bed with the curtains closed in a communal room and I had no time to be able to process that."
'Very traumatic experiences'
It was not a criticism of the NHS, she said, explaining "that's the constraints they're working with".
Dr Nav Masani, a consultant cardiologist at University Hospital of Wales in Cardiff, agreed the right environment and support can have a big impact.

Consultant cardiologist Dr Nav Masani says a patient's surroundings can help them deal with trauma
"We know that individual patients and their families have gone through very traumatic experiences on cardiology wards," he said.
"Sometimes they have come back to us and reflected that the one thing that stuck in their mind was something to do with the environment."
His team and patients have use of one of the rooms renovated by Daring to Dream, of which he is also a trustee.
As a clinician who predominantly treats young adults, he is aware of their specific needs.
Increasing fear factor
"They might have to take more time off school, or get peer group pressure that you simply don't have as an older age group," he explained.
"They may miss out on activities that their friends are able to do," Dr Masani said. "And some of them without a doubt have to face the sort of increasing fear factor of having to come back into hospital repeatedly.
"So to do that with a long-term health condition requires an increasing focus on emotional health and wellbeing."
One of his congenital heart failure patients, Amy Penn, decided to hold a charity ball to highlight the issue.

Amy Penn held a charity ball to raise awareness about emotional health before her death
Amy died in June last year, aged 21, but the ball she started has continued.
"Amy was very resilient," said her mother, Hayley Penn, from Newport. "But it does take its toll."
Heart surgery left Amy with scars, but in later years other procedures were harder to cover.
"Amy also needed mouth surgery and I think over the years, through all the other treatment for her heart condition she just got on with it," she said.

Hayley Penn says the mental health support her daughter Amy got was a "massive lifeline"
"But her mouth surgeries were the worst," Hayley said. "That got Amy down - because there were physical changes - her features, her face - and they were very painful interventions.
"She knew her smile changed," she explained.
"But the mental health support that she received from her cardiology team, her friends and the Youth at Heart group was a massive lifeline," Hayley said.
The congenital heart charity, external can send flowers or deliver a favourite meal ahead of an operation.
Barbara Chidgey, the founder and chair of Daring to Dream, said feedback from patients they support highlighted this as a big theme for many young patients.

Barbara Chidgey founded a charity aiming to help the wellbeing of patients
"Young adult patients have particular emotional health and wellbeing needs," she said. "I can't imagine what it would be like being a teenager with a serious, chronic condition, when all of your friends are able to go out clubbing.
"So we facilitate wellbeing activities and services, in and out of hospital, as well as transforming spaces like the quiet rooms in hospitals where a lot of tough conversations happen," she said.
The Welsh government said it was "acutely aware of the challenges facing people living with chronic and long term illnesses".
"We are are working with the NHS to ensure all patients are supported. Our planned care recovery plan will help people manage their condition, both before and after treatment.
"We have increased funding to improve access to a wider range of psychological therapies to help support people's emotional health and wellbeing," it added.
"We are also developing new standards and guidance on social prescribing which is already playing a role in boosting peoples wellbeing in Wales."
Related topics
- Published17 March 2021

- Published23 August 2021
- Published5 June 2019
