NHS Wales: Betsi Cadwaladr patients ask boss if it's safe
- Published

Nick Lyons said it could be "years" before some of the issues at Betsi Cadwaladr were fixed
Repeated failings at a troubled health board have left people asking a top boss if it is safe to be treated there, he has admitted.
Betsi Cadwaladr health board has been rocked by a series of damning reports and even had to be overseen directly by the Welsh government for five years.
Medical director Dr Nick Lyons said there was "a risk" patients could be reluctant to seek help as a result.
"Amazing" staff also feel "frustrated" and under-appreciated, he added.
'Sometimes you feel like your best isn't good enough'
While Dr Lyons insisted the vast majority of patients receive good and effective care, he had people asking him: "Is it safe for me to be treated here Dr Nick?"
"And yes it is, even though there are some significant issues to be addressed."
He conceded it could be "years" before some of those issues were fixed, adding: "I must take responsibility and say sorry for those people for whom they don't get the urgent care they should expect".
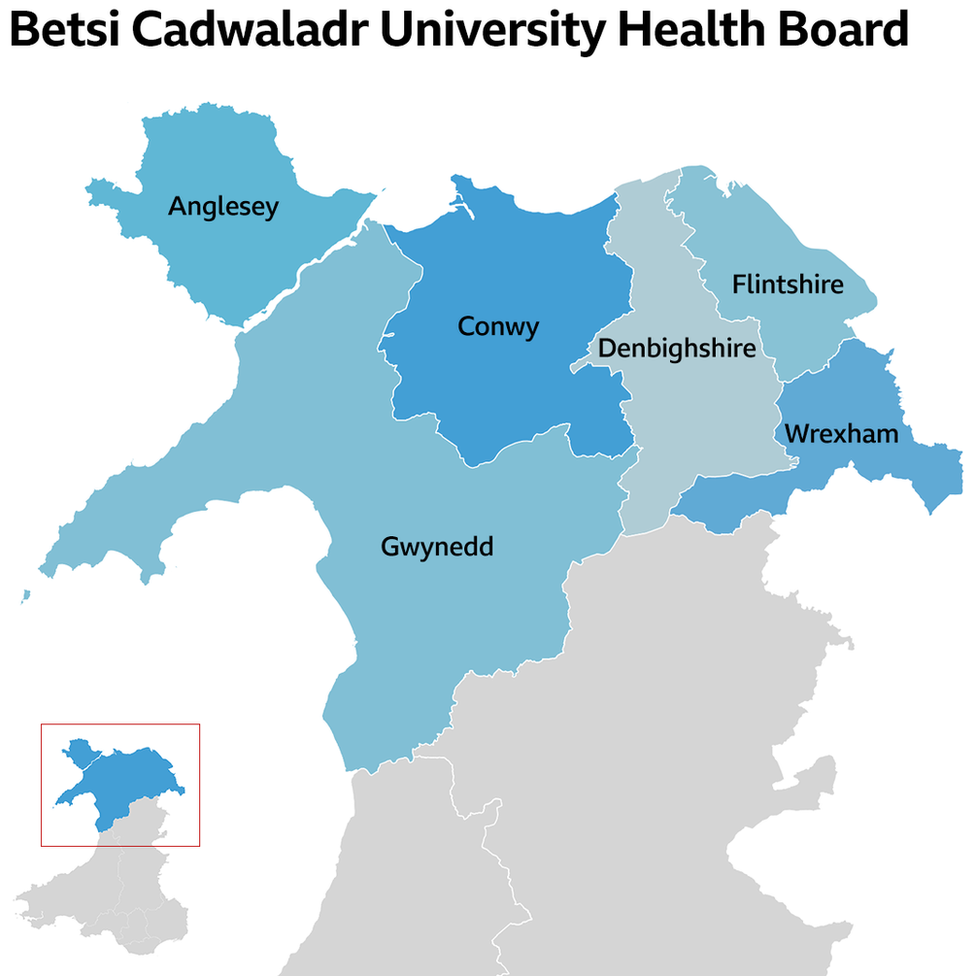
Betsi Cadwaladr health board has 700,000 people living in its area

Staff shortages were a contributory factor in many of the problems highlighted in reports, with Betsi's reputation making it harder to attract staff to fill vacancies.
GPs, A&E and oncology and cancer services are all areas with particular shortages, while vascular services, external had six out of nine full-time consultants with temporary doctors filling the rest, which costs more money.
In September, 6.5% of Betsi's wage bill went on agency or temporary staff - about £13.9m.
Another side effect of the health board's continuing struggles is the knock-on effect on staff.
Dr Lyons said staff were not always appreciated and their hard work was not always recognised.
Gemma Beck, a radiographer at Ysbyty Glan Clwyd cancer treatment centre, agreed. Her team worked throughout the pandemic, but she soon noticed some colleagues were struggling.
"Some colleagues couldn't see their families and some were living in caravans. They were isolated and saw nobody apart from at work."
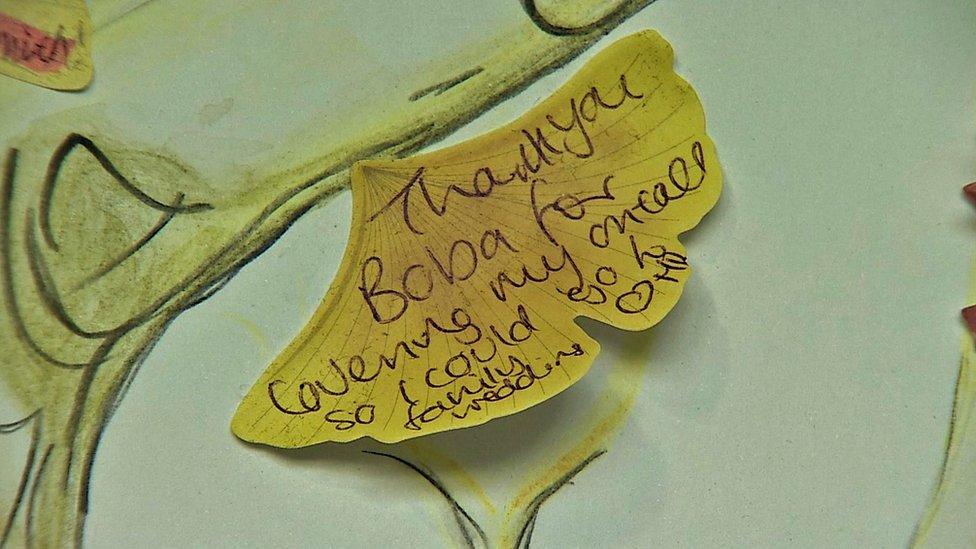
Gemma Beck's appreciation tree allowed staff to post kind messages to one another, in a bid to boost morale
Ms Beck went about raising spirits by designing an "appreciation tree" so staff could post thank you messages to each other.
She also spent hours on top of her shifts producing a monthly staff newsletter to spread good news to "put a smile on people's faces".
Subsequently, she was nominated for a staff "going the extra mile" award but still feels the problems facing the NHS and the related negative publicity makes staff feel under-valued.
"I don't tend to read articles because it gets me down.
"We're working so hard every day, but you're not getting the recognition you deserve because you keep reading negative things online.
"Sometimes you feel your best isn't good enough, which is a shame."
One of the health board's top priorities is to improve conditions at A&E at Ysbyty Glan Clwyd in Bodelwyddan, Denbighshire.
A highly critical inspection report in March spoke of "excessive" delays, with a follow-up report saying there was "a significant risk" to patient safety.
Ysbyty Glan Clwyd, Wrexham Maelor Hospital and Ysbyty Gwynedd A&Es are consistently among the worst performers in Wales for patients having to spend more than four or 12 hours waiting.
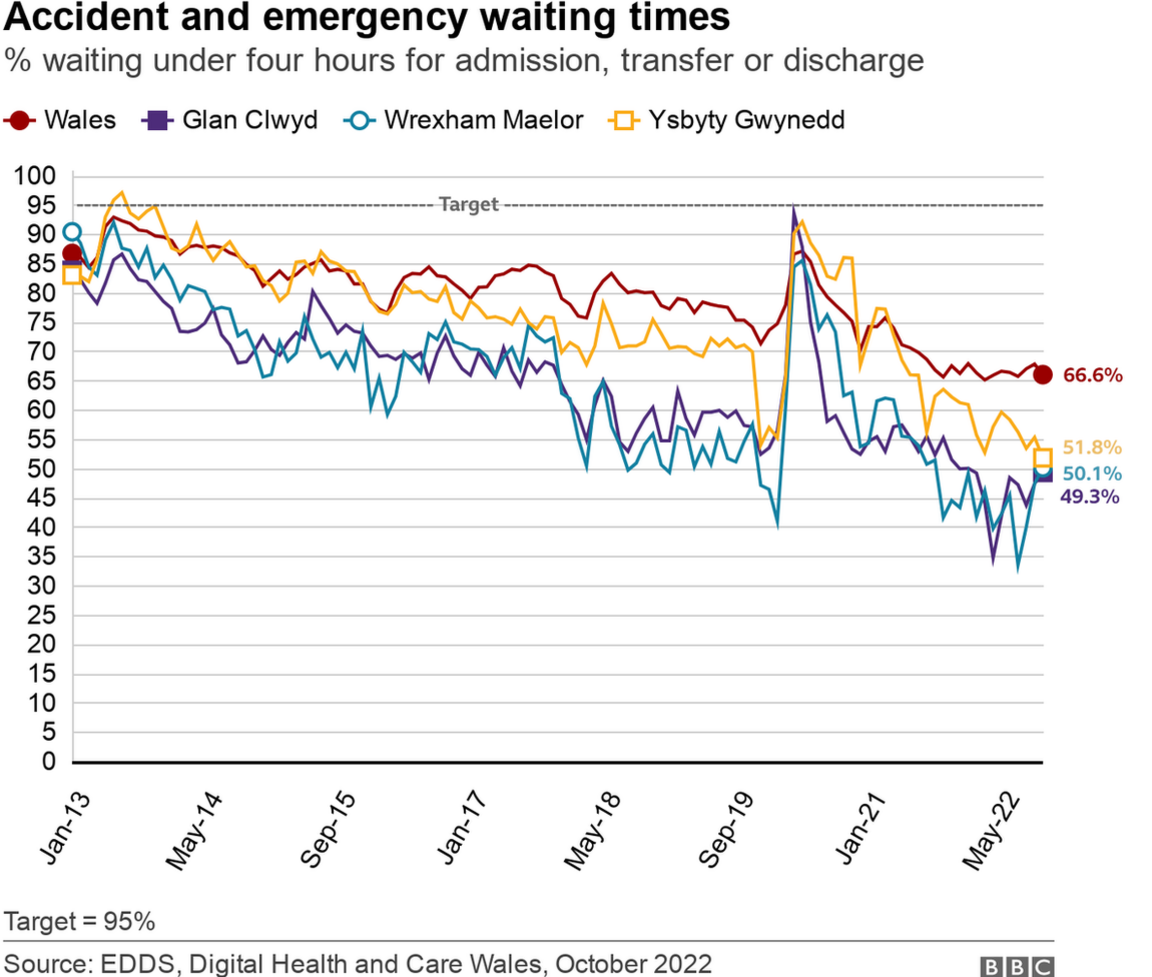

Gaynor Thomason, who is charge of the team whose job it is to turn things around, said there were about 300 people in hospital who were fit to be discharged but were still waiting to leave.
"People were trying to work in a crisis situation and fix things without any headspace."
Ways they have begun to tackle A&E waiting times include having senior nurses at the front door to "ask the right questions so we can identify those that need the most immediate care".
However, Ms Thomason said changing the wider system was "going to take a long time" and those waiting six or seven hours would be offered a tea and a sandwich.

What is the history of Betsi Cadwaladr health board?
Established in 2009, Betsi Cadwaladr became the first and only health organisation to be put entirely in "special measures" - the highest level of Welsh government oversight, in 2015.
Even after they were lifted, big problems remained and last summer one of its three big hospitals, Ysbyty Glan Clwyd had serious concerns raised about its vascular services and A&E.
It will remain in "targeted intervention" for the foreseeable future.
It has also gone through nine chief executives in 13 years.

Staffing issues across the NHS are a key factor in longer waiting times
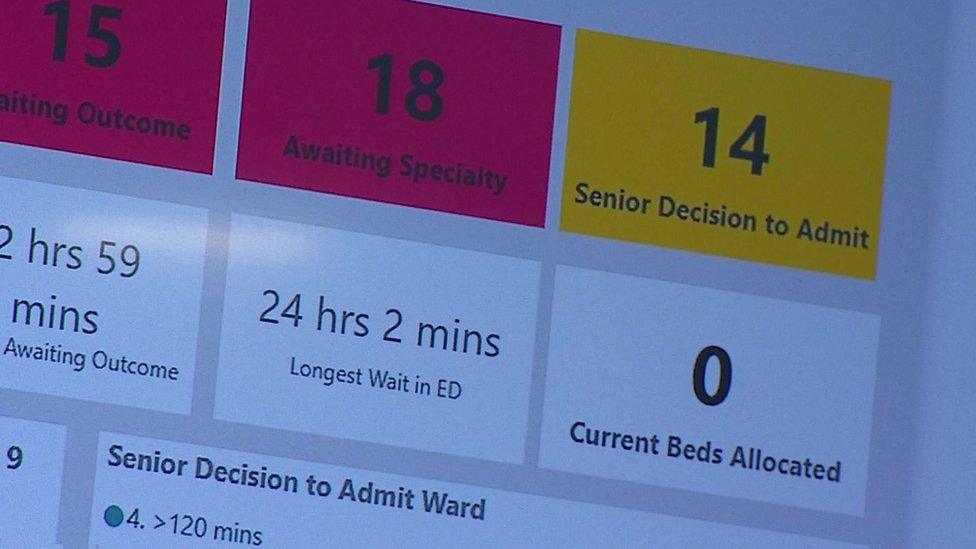
On a recent visit to Glan Clwyd Hospital, BBC Wales found seven ambulances queuing outside A&E - one of which had already been waiting for eight hours and 51 minutes to transfer their patient.
Another screen showed there were 58 patients, with the longest wait being 24 hours and two minutes.
Staff said there could be as many as 120 patients waiting on busy days.

Freeing up hospital beds is one of the struggles the health board faces
Clinical site manager Martin Farr said these long waits were caused by too few free beds on hospital wards to move patients to, while a lack of social care in the community slowed things down even further.
Health board and local authority staff in Ruthin attempt to stop unnecessary trips to hospital and speed up discharges, two of the health board's main challenges.
They hope with enough support from community nurses, GPs and social care staff, people's beds at home can work like wards beyond hospitals, increasingly the number of available beds.
"The last thing we want to see is our patients to be sat in ambulances for hours on end when we could put something in place to help them stay at home," said Lisa Orhan, community matron for Denbighshire.
- Published3 February 2022

- Published20 May 2021

- Published16 February 2022

- Published1 September 2022

- Published24 November 2020
