A&E wait: Frustration over disabled man's 48-hour ordeal
- Published
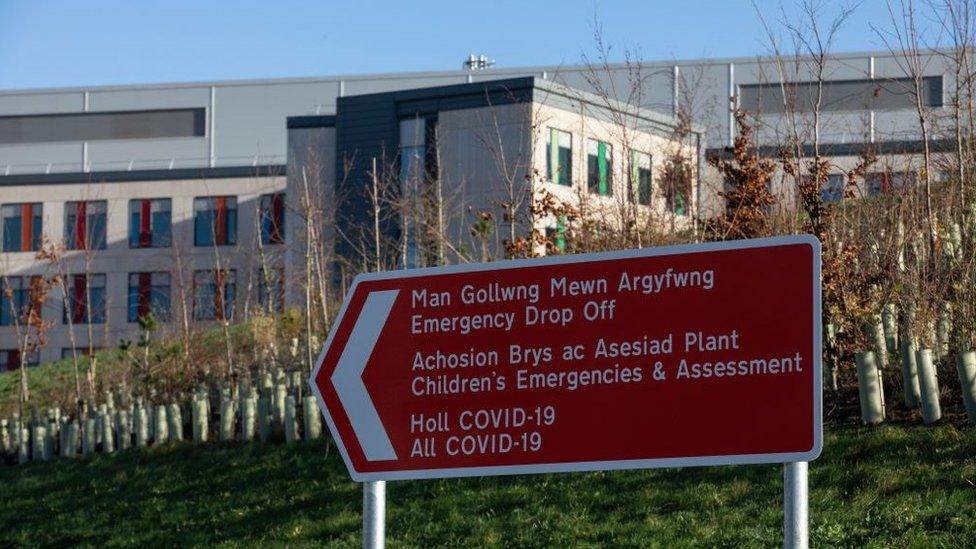
Aneurin Bevan health board says delayed discharges and winter viruses have led to longer waits at A&E at the Grange Hospital in Cwmbran
A care agency boss has described the NHS as "a joke" after a disabled man was forced to wait for 48 hours in A&E.
One of David Williams' clients, who has severe epilepsy, had been taken to the Grange Hospital near Cwmbran, Torfaen, complaining of chest pain.
Mr Williams said he had to wait in a chair with no food for 36 hours.
Aneurin Bevan health board said delayed hospital discharges and winter viruses had led to longer waits at A&E.
Mr Williams, the responsible individual and director of Prestige Care Agency Services, said the NHS was a "failed system".
In November, Healthcare Inspectorate Wales' (HIW) said urgent improvements were needed at the hospital, which opened only two years ago.
Recalling the incident on 5 December, Mr Williams said: "He was held for 36 hours in a chair and for about 12 hours in a side room whilst they tried to admit him into hospital for tests.
'Very, very frustrating'
"He didn't understand really what was happening, he wouldn't have been comfortable.
"How we as a company funded by local authority end up with the ultimate responsibility in that situation was very, very frustrating."
He said one member of his staff stayed with the man for more than 24 hours before handing over to another member of staff.
He added the patient missed out on food and drink as he was asleep each time the food trolley went by, and when he was awake, staff were too busy to bring him any refreshments.
Not only this, his staff were unable to leave his side and get food and drink for themselves.
"I think next time it happens we'll certainly be sending down food and drink because it's a long time just sat there waiting for something to happen, being hungry and thirsty," he said.
The incident prompted him to write to the Western Mail newspaper, where he described the NHS as "a failed system" and "a joke".
But he does have some sympathy for hospital staff.
David Williams' employer provides supported living services to 17 people across five homes in Torfaen
"A&E is carnage, they're rushed off their feet," he said.
"I don't think it was any fault of the hospital, I think it's a fault with the system."
He added: "There's a fear of destroying the myth that the NHS is fantastic and the best in the world... I think it needs a fundamental shake-up."
Aneurin Bevan University Health Board said: "We are sorry that Mr Williams is unhappy with the care that his service users have received and the long waits they experienced."
It said it was experiencing "unprecedented demand" for its services.
"With high numbers of winter viruses spreading throughout our local communities, this is putting severe pressure right across our system, which has, unfortunately, meant that patients are waiting longer to receive care in the emergency department than we would want," it added.
It said its hospitals had at least 300 patients who were medically fit for discharge but were awaiting some form of support at home before they could leave hospital due to the significant challenges facing social care.
"This results in a delay for these patients returning home, which, in turn, is affecting the overall flow of patients through our hospitals."
It asked Mr Williams to contact the health board directly to discuss any concerns.
Mr Williams, whose company provides supported living services to 17 people and employs 40 staff across five homes in Torfaen, said situations like this were leaving people working in his industry with the "horrendous decision" over whether taking a service user to A&E was in their best interest.
"You have to make these unqualified decisions really, which is pretty uncomfortable I have to say," he said.
He said recently when an elderly man fell out of bed, staff called for an ambulance and were told there was not one available.

Grange University Hospital opened two years ago
"The guidance says you leave him on the floor. You cannot leave an 88-year-old man on the floor for hours and hours so in the end I said 'just pick him up'," he said.
"We're at the point where we're having to make decisions which we shouldn't be making."
He said if services like his could access GPs over Zoom where they could actually see the patient it would be a big help, adding: "But I guess it's all about the money at the end of the day."
The Welsh government said: "We were sorry to learn about the patients' experiences and we are supporting the health board and partners in providing better outcomes for patients who need access to urgent and emergency care."
It said the health board was receiving an additional £3m annually as part of an investment of £25m it was making to transform urgent and emergency services across Wales.
Mr Williams believes the solution to ending long waiting time at A&E is a properly funded care system.
"The care sector is not funded properly," he said.
"The care sector is largely a fragmented private industry which has organically grown to meet the need of society."
Mr Williams said although there was a "lot of pleasure in helping somebody who's got a disability", until carers received better pay there would always be a problem with recruitment and retention in his industry.
"I don't think £9.90 or £10 an hour is enough for the level of responsibility that they have," he said.

Aneurin Bevan health board said delayed hospital discharges and winter viruses had led to longer waits at A&E
"We have a lot of service users with choking risk, it's a constant worry, you have to be watching people all the time.
"It never lets up - there's no Christmas, there's no Easter.
"When people can go and work in retail for more for almost zero responsibility by comparison we see people going in that direction," he said.
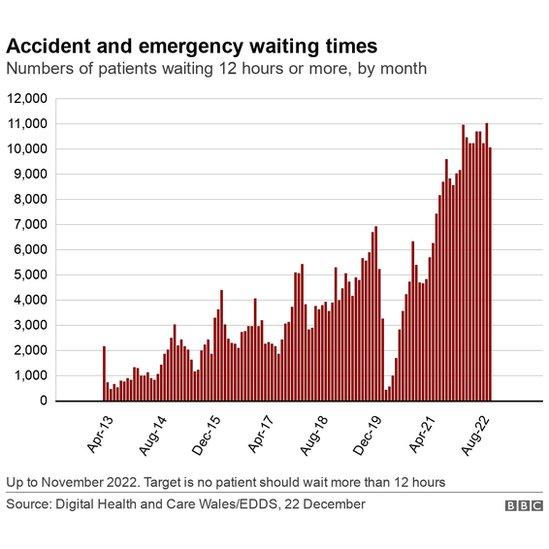
What do the stats tell us?
In November, 67.3% of people were seen within four hours at A&E, higher than October but still significantly worse than the pre-pandemic performance. The target, which has never been met, is 95%.
The month also saw more than 10,000 people waiting more than 12 hours in A&E; the target is that no-one should wait that long.
Meanwhile, ambulance response times were the joint worst on record - with only 48% of "red" life-threatening calls arriving within eight minutes.
Although the number of hours lost to handover delays outside A&E units had improved on the previous two months, 24,250 hours were still "lost" with ambulances unable to hand patients over at emergency units beyond the 15-minute target time.
So far this year, more than 260,000 hours have been lost.
Related topics
- Published17 November 2022

- Published28 September 2022
