NHS Wales budget: What's behind the overspend
- Published
Organisations which run Welsh hospitals have been put under more scrutiny in the wake of growing deficits.
A double whammy of inflation and having to fill rotas because of vacancies have left health boards in the red by nearly £250m in the most recent three-year financial cycle.
There are fears that will get much worse by next spring, with annual deficits alone close to £850m.
So what are some of the main reasons?
Here were try to answer some of the questions.
How bad are the overspends?
To the end of March 2023, the deficits for the main Welsh health boards had reached £151.9m for that single year.
But these are now expected to be much more by the end of March 2024.
Health boards were already working to planned deficits of nearly £650m - but that could reach nearly £825m if the worst fears are realised.
NHS bodies are required to plan financially over a three-year cycle.
Measured over the latest three-year period, overspends reached £247.8m across Wales by March 2023.
The highest are in west Wales, with a deficit of nearly £109m in Hywel Dda - which covers Carmarthenshire, Pembrokeshire and Ceredigion - alone, followed by £46.8m overspending in Swansea Bay.
Both these health boards have been consistently in deficit since before the Covid-19 pandemic.
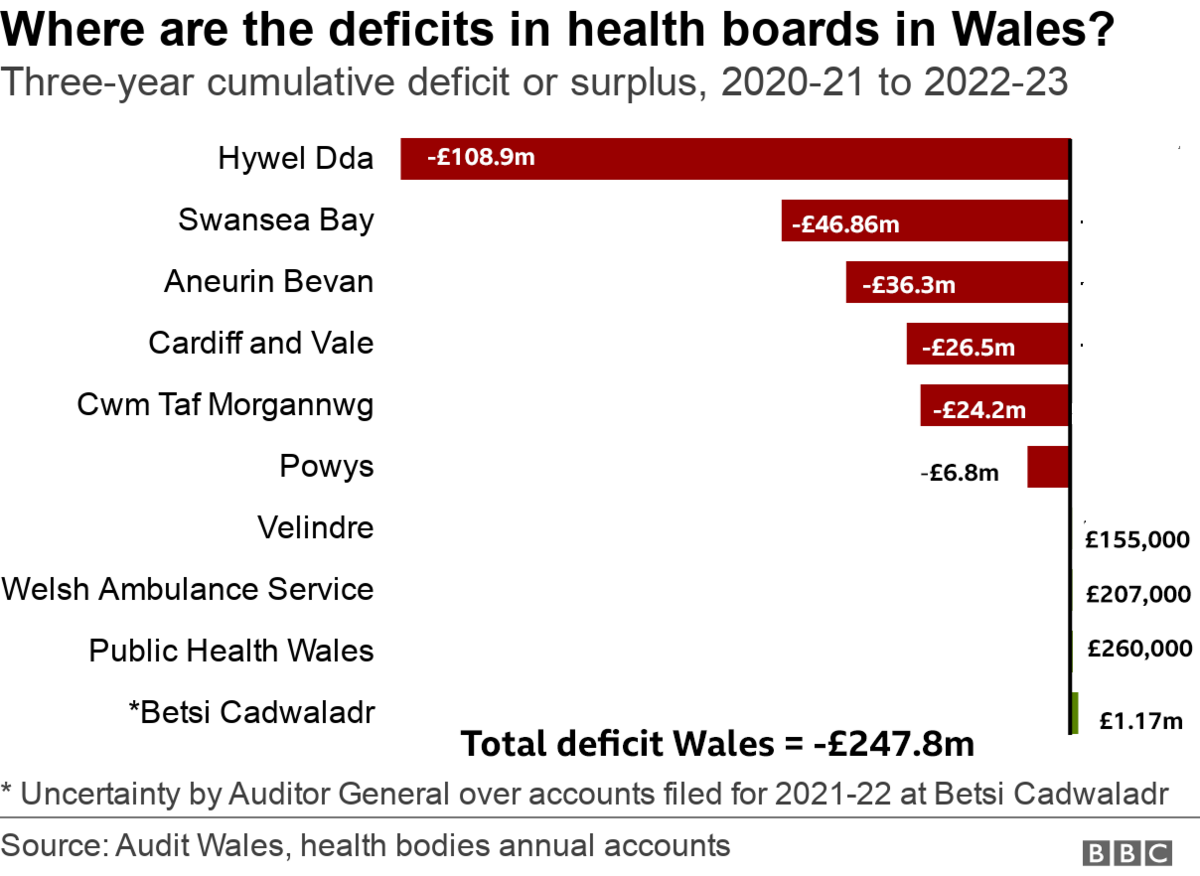
The only main hospital health board without a deficit is Betsi Cadwaladr - but the Auditor General is not happy with the accounts here either due to "uncertainties", so its finances too are under the microscope.
What has been the impact of inflation?
NHS Wales is not immune from rising costs like any of us - and as Wales' biggest employer and organisation it faces paying more for running things so these numbers will be big.
Already by the end of 2022-23, despite getting an extra £131m in funding, rising inflation meant it felt like a reduction - with a 4.9% real terms decrease in funding.
The picture is even worse this financial year as inflation really bites in areas like energy costs to run hospitals and the rising costs of drugs.
If we look at Glangwili hospital in Carmarthen, its energy costs have risen from £5m a year to £14m. It is an old hospital and they still rely on oil.
Drug costs have also seen a "huge increase". For example, the cost of omeprazole - a common medicine to deal with stomach acid - has jumped from 80p a packet to £2.80 in the past 18 months. Across the whole health authority that can add £500,000 to costs.
The cost of some other medications have gone up three or four times in only weeks.
Lead pharmacist at the hospital, Owain Williams, said: "It can be difficult but it's important for patients to know we won't be stopping the medicines they need but looking at the most cost effective product, perhaps switching to an alternative product brand which is clinically effective but not costing the NHS as much."
The health board said there were long term pressures because people were living longer and then short-term staffing and inflationary pressures, as well as demand rising for treatment and tackling waiting lists.
Huw Thomas, Hywel Dda finance director, said: "There's a gap between what we are spending to sustain the needs of patients and balancing that with the needs of the tax payer to demonstrate value for money."
In this current financial year, it were planning for a deficit of £113m but the current trajectory was far higher.
"It's a perennial challenge," he added.
What about staff costs?
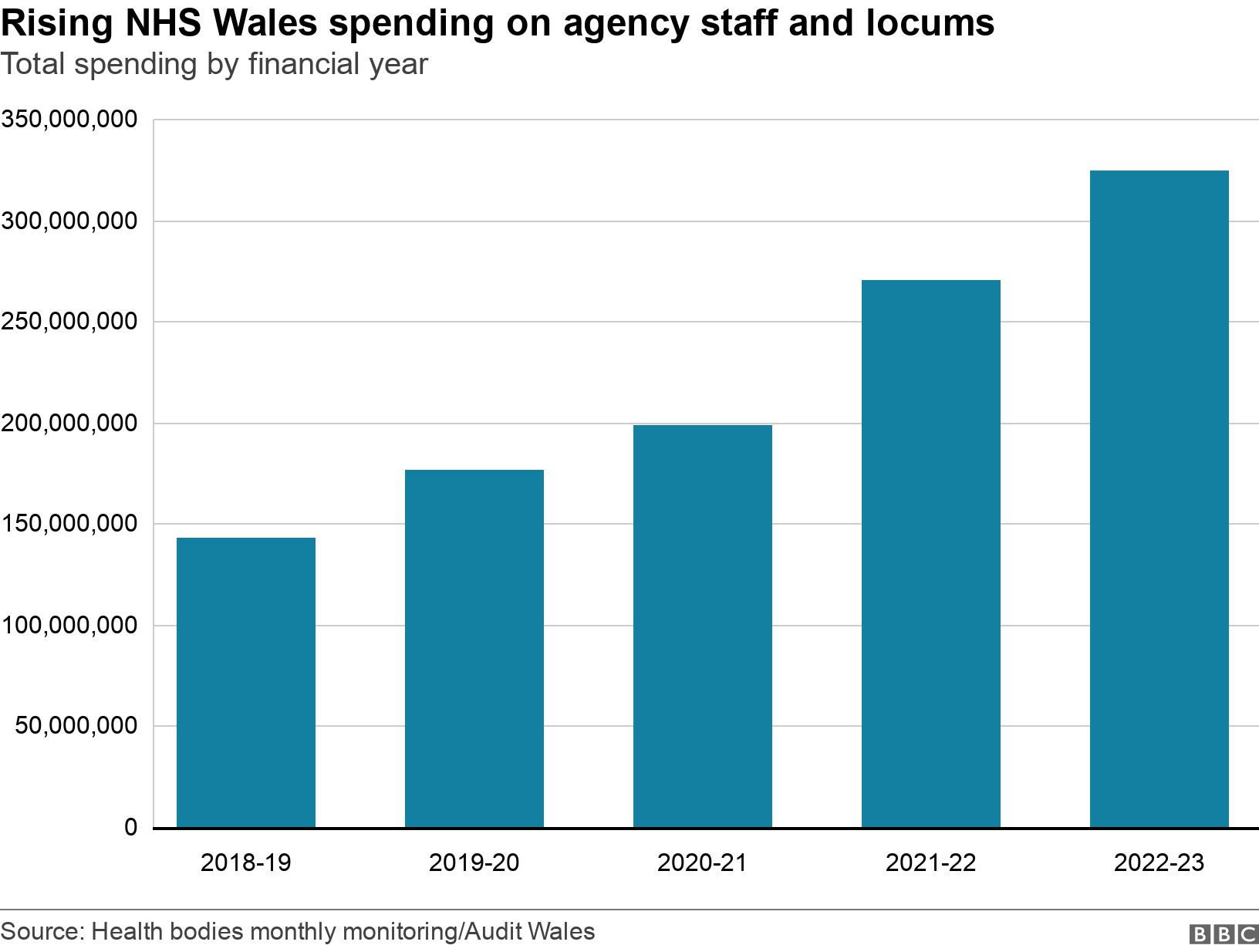
Across NHS Wales, spending on agency and locum staff has more than doubled in four years to close to £325m in 2022-23.
More than two-thirds of this was due to staff vacancies.
That is the experience too at Hywel Dda health board, which spent £38m on agency staff. There are 100 vacancies altogether although it is hoped a recruitment drive abroad will stabilise some of this.
The health minister on Thursday gave Senedd members a "guarantee" that the number of agency staff would fall, with permanent staff recruited to replace them.

GP Dr Llinos Roberts is facing rising costs as a small business but also rising demand as patients developed complications after two years of Covid
Has Covid had an impact?
"What we saw over the first two years of Covid was a push advising patients not to visit the surgery for people and not to leave the house," said Dr Llinos Roberts, a GP near Cross Hands, Carmarthenshire.
"That resulted in all the other illnesses and diseases which were still happening being pushed to one side and people were reluctant to come for advice because they felt it wasn't wise or might pose a risk.
"All those chronic diseases that we would have liked to be reviewing regularly - we might not have seen those patients over two or three years but now we're seeing them again.
"Perhaps they've developed complications in that time, where we could have prevented them if we'd manage to see them."
Waiting times have also increased the pressure on GPs, while the health service as a whole is dealing with the backlog - adding to financial pressures.
What are escalation levels?
At least twice a year, officials the Welsh government, Audit Wales and Health Inspectorate Wales meet to discuss how each health board is performing.
Each is given one of four stage escalation levels, external - which start at routine, when things are business as usual.
"Enhanced monitoring" is the second level of scrutiny.
"Targeted intervention" is the third level - promising even more scrutiny and action to strengthen the capabilities of the health board to drive improvements.
The fourth level is special measures which can see the health minister step in to shake-up those leading the health board.
We are now at the stage when the seven main health boards are all together on at least the second level of scrutiny, or above.
Will this affect patients?
Those running the hospitals want to point out they will not stop treating patients or stopping some medicines or treatment.
This financial issue is in part from having to address the waiting list backlog, a sign that hospitals and GPs are trying to get back to normal after Covid.
But even doing the same as they were doing last year costs much more.
What can be done?
Those keeping an eye on public money spent in Wales say despite the challenges, NHS health boards still need to do more to help.
There was too much concentration on looking at one-off savings - putting off spending rather than looking for efficiencies.
Adrian Crompton, Auditor General, last week said there needs to be a more strategic approach, external and also for efforts to tackle spending on agency staff.
Darren Hughes, director of the NHS Confederation in Wales, said: "Even organisations who are doing the best job of managing demand and their finances are really struggling to make ends meet."
He said it was not about the NHS doing less but the whole of the public sector working to help people stay well.
"But if we can keep people well, keep people healthy longer we can provide a better standard of care. We need to do something about the demand at the front door of of hospitals to enable us to deliver."
Every minister in the Welsh cabinet has been asked to find savings from their budget before they meet - but easy savings will be hard to find, considering how much of the Welsh budget is spent on the NHS.
A big overspend could make the whole financial position of the Welsh government more precarious.
The NHS in England is facing similar issues, which the UK government will need to address. If it decides to bail out the NHS in England in the autumn statement, equivalent money would then come to Wales.
Related topics
- Published13 September 2023

- Published20 October 2022

- Published5 December 2022

- Published11 August 2023
