Sexual health: Social media users warned about STI myths
- Published

Chlamydia and gonorrhoea infections are at a 10-year high
A lack of education is making young people susceptible to social media sex myths, a youth charity has warned.
Amy Stuart-Torrie, from the YMCA, said she had met young people who believed washing after sex could prevent sexually transmitted infections (STIs).
She said another myth was that drinking out of bottles made from BPA plastic could prevent pregnancy.
Public Health Wales (PHW) figures, external show chlamydia and gonorrhoea infections are at a 10-year high.
The majority of cases are in the 15-24 age group.
Diagnoses of syphilis and herpes have also increased since the end of the Coronavirus pandemic, according to the figures.
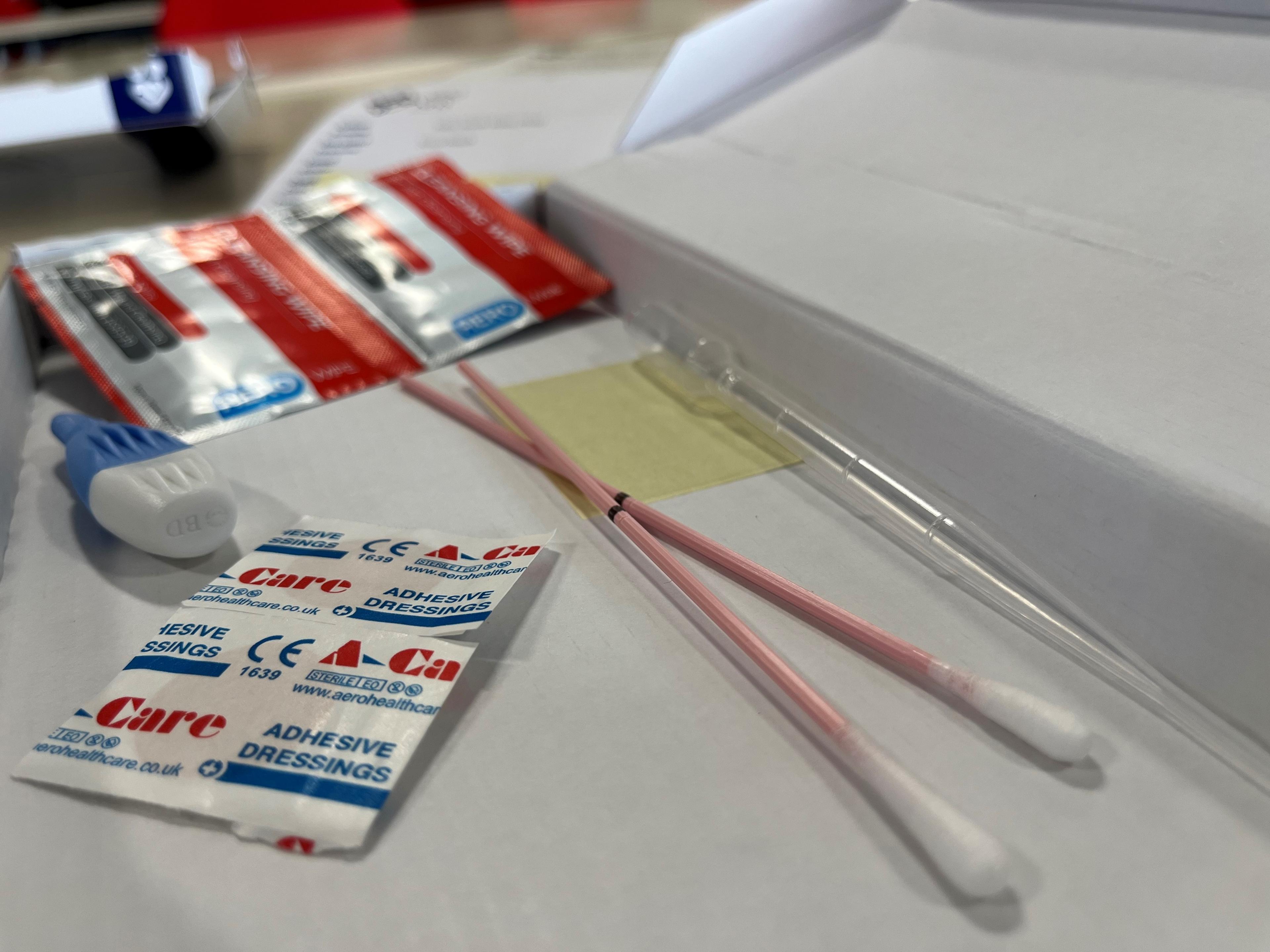
PHW said testing was also at a 10-year high, due to an increase people taking up free at-home testing.
Amy, from the YMCA's Healthy Relationships service, said the jump in STIs was "alarming" but that due to gaps in education, exacerbated by the pandemic, "huge chunks of information have been missed".
She said she sometimes saw a "blasé" attitude to STIs, particularly from young men.
"They're adamant that there's no health implications to chlamydia," she said.

Amy said misinformation can be easily be spread on social media
Other misconceptions she has heard include that you could become immune to STIs once you've had them once, or that they will go away by themselves.
Her service runs the c-card scheme, external, where 13-25 year olds can get up to 10 free condoms a week as well as sexual health and relationships advice.
She said speaking about sex and STIs was not aimed at scaring people.
"The more young people know what's out there, the better informed they are, they can make good decisions themselves to keep themselves as safe as possible," she said.
Dr Darren Cousins, who works as a sexual health consultant in the Cardiff area, said the figures showed "people may be making up for lost time that they had during the Covid times".
"For many reasons, for many things, [that] is a good thing but unfortunately for us means we will see more sexually transmitted infections," he said.
"Partly that's because things like HIV have been much easier to treat so people are less scared of infections than they may have been before," he said.
"Condoms are expensive so that may have an impact as well."
PHW figures show chlamydia and gonorrhoea infections are at a 10 year high
Unlike England, Wales has universal free test-at-home kits, external, which Public Health Wales attributes as a key driver behind the recorded STI rise.
Dee Whitnell, 24, is a qualified sex educator who runs online sex and relationships education accounts on social media under the handle @s3xtheorywithdee.
They said online testing kits avoided "awkward sexual health clinic visits where someone may notice you, or you have to chat to a stranger about your sexual experiences".
Dr Darren Cousins agreed.
"It's convenient for people, they don't have to take half a day off to sit in a clinic room," he said.
He urged people who have had unprotected sex to order a kit.
"There are long-term consequences of untreated STIs so things like sub-fertility, chronic pelvic pain and so it's better that we test these infections at an early stage," he said.
'A vibe killer'
Research by the Sexual Health Research Network, external showed post-pandemic only 41% of year 11 students in Wales reported using a condom.
Amy pointed to "peer pressure" creating a reluctance around young people using barrier methods of contraception.
"They don't like the way it feels, or they're too tight or they're a vibe killer," she said.
She said many young people also turn to porn to find out about sex, which rarely depicts condom use.
She said some young people had experienced stealthing, illegally removing a condom during intercourse without consent, so wider conversations about proper condom use were also important.
However she said "hundreds" of people had signed up to the c-card service, while there was a waiting list for their relationships service showing the desire for education.

Dee (second from left) said many LGBTQIA+ individuals did not realise they need to use barrier contraceptives
Dee Whitnell agreed young people were going online to "fill in the gaps that their in-class sex education has missed", especially when it came to different sexualities and gender identities.
"LGBTQIA+ individuals are heavily left out of the conversation, meaning many don't realise that they need to still use barrier methods even if they or their partners can't get pregnant," they said.
"Everybody deserves access to inclusive and comprehensive sex ed that reflects their experiences and without that, young people can find themselves in dangerous or very uncomfortable situations."
They added that there was a responsibility for sex educators to "ensure their resources are accessible for all, accurate and representatives."
Recorded cases of STIs on the rise
The PHW data showed between 2021 and 2022 there was an increase of 22% in chlamydia diagnoses, and a 127% increase in gonorrhoea.
There was also a 14% increase in syphilis cases and 18% in herpes diagnoses over the same period.
The research also recorded a 56.5% reduction in HIV cases over the last 10 years.
Fitting of long acting reversible contraception (coils and implants) in sexual health clinics has declined by 22% since 2019.
PHW noted that abortions had increased by more than a third (34%) in the five years up to 2021.
Related topics
- Published28 September 2023

- Published15 September 2023

- Published28 July 2022
