Ebola in DR Congo: Fear and mistrust stalk battle to halt outbreak
- Published
The body bag saving lives in DR Congo's Ebola outbreak
There can be few greater challenges than tackling a lethal epidemic.
But imagine trying to do so in a conflict zone ravaged by extreme poverty, insecurity and poor communications amid a population where health workers are feared and distrusted.
Yet that is the reality of Ebola in the east of the Democratic Republic of Congo, where more than 1,500 people have lost their lives from the virus in the past year.
In the city of Butembo, in North Kivu province, I see how local and international medical staff and charities are trying to combat the disease.
Essentially, it is a gruesome game of whack-a-mole that appears all but impossible to win. It works like this:
The morning I was there, news came through that a woman had died of Ebola.
Staff from the World Health Organization (WHO), the UN-funded agency, rushed to the scene and set up a pop-up vaccination centre. What this means in practice is a few trestle tables under a number of tents.
Then, members of the dead woman's family, her friends, her neighbours are identified and are asked to be vaccinated. Afterwards, their wider contact group are vaccinated too in the hope this double ring of protection will stop the virus in its tracks.

What is Ebola?

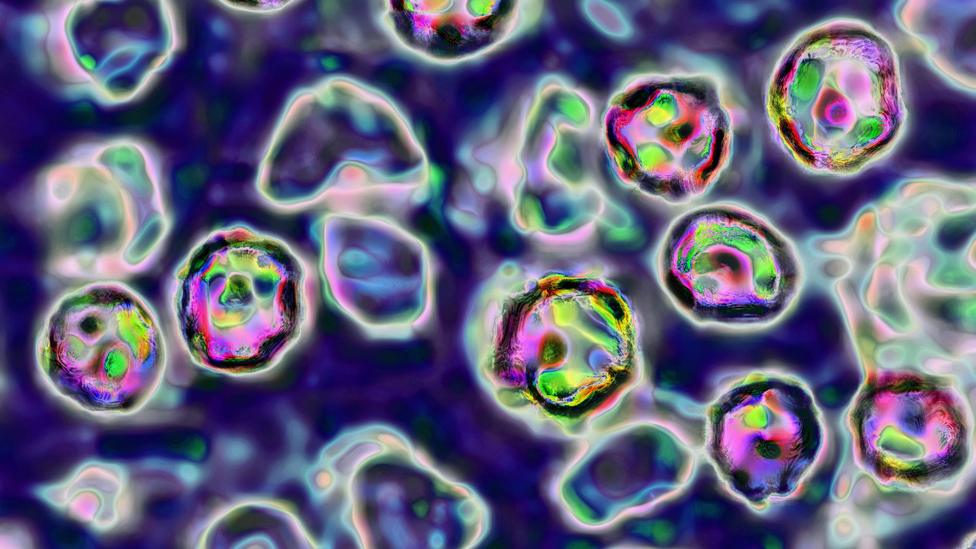
Ebola is a virus that initially causes sudden fever, intense weakness, muscle pain and a sore throat
It progresses to vomiting, diarrhoea and both internal and external bleeding
People are infected when they have direct contact through broken skin, or the mouth and nose, with the blood, vomit, faeces or bodily fluids of someone with Ebola
Patients tend to die from dehydration and multiple organ failure

These vaccination centres are funded in part by the British government. The UK's International Development Secretary, Rory Stewart, was there to see for himself what his department is getting for its aid budget.
And they are clearly making an impact. But only up to point, for there are challenges that this model struggles to overcome.
Many Ebola deaths are never reported. Decades of conflict have led to widespread mistrust of the authorities and this has an impact on the disease spreading, according to authors of a recent report.
Some deny the disease exists, believing it to be a poison invented by the international community to traffic body parts. Others do not trust trained medical staff to look after the sick.
Then there are those who simply do not want their loved ones snatched from them, sealed up in a plastic body bag and buried anonymously by someone else.
This matters, because the corpse of an Ebola victim is most contagious at the time of death. So if families are busy cleaning the body as part of customary burial rites, they are all spreading the contagion and almost certainly condemning themselves to a wretched death.
Even if a death is reported, that does not solve everything. Not everyone agrees to be vaccinated or provide information about their wider contact groups. There is little the medical staff can do to force them to hand over names and addresses.
Some people, even if vaccinated, still contract the disease. It seems inevitable that there can never be enough quick response teams to match the number of Ebola deaths. So the medical staff sometimes come too late and the virus will have spread.
Some simple techniques can help prevent spread of Ebola
Vaccinations have undoubtedly had an impact. After more than 11,000 died in the outbreak that hit Guinea, Liberia and Sierra Leone earlier this decade, external, there have so far been fewer deaths in the Democratic Republic of Congo.
But for all the lessons learned and the huge amount of resources thrown at this outbreak, it continues to spread.
Containing the virus
Butembo is a trading centre with a "highly mobile population", says the WHO, external, that comes from elsewhere inside the Democratic Republic of Congo as well as regional neighbours Rwanda, Uganda and Kenya.
There are fears the virus could spread south to Goma, the regional capital of North Kivu and a major transport hub for the country and region. If this happened, the outbreak could be transformed.
More than one million people are packed into Goma's dense urban sprawl on the shores of Lake Kivu, meaning the disease would spread fast and be almost impossible to control.

I visit the border with Rwanda, where tens of thousands of people cross each day.
Everyone passing through must wash their hands in chlorinated water, have their temperatures taken and answer questions about where they have been and their contact with Ebola sites.
There are public information songs and announcements about how to prevent the spread of infection.
So far, Ebola has crossed only one border - into Uganda - but luckily it failed to spread. But if it crossed into Rwanda, the consequences would be significant.
Apart from the potential medical consequences, there would be an economic impact.
If the border were to close, thousands of small traders would lose their livelihoods, adding to existing poverty.
And if left open, there could be huge population movements across the region. So, stopping the spread to Goma is a priority.
Treating Ebola in the DR Congo warzone
With Mr Stewart, I visited an Ebola treatment clinic at Goma hospital that is being partly funded by the British government. There is also another clinic being built on the other side of town.
But the minister clearly believes the levels of preparedness need to be stepped up and is urging countries like France, Germany and Canada to provide badly needed resources.
He also wants the World Health Organization to formally declare this a global health emergency - a technical definition - that would make it easier to raise money internationally.
'Secret sums'
At the moment, the biggest donors are the United States and the UK. How much they are giving is kept largely secret because there is a fear that bandying about figures of millions of dollars would increase attacks on health workers.
Such is their suspicion of a world that largely ignored their country through decades of civil war that some Congolese believe the international community is using Ebola to make money. And they hope that some of the health workers and aid staff might have some of that money themselves.
The fundamental question now for the outside world is what lessons they can learn from this outbreak. For few believe that Ebola will be defeated entirely.
Many reckon that viruses like this in future will have to be managed rather than eradicated.

Family members place leaves on the grave of a deceased relative who died from Ebola in Butembo
- Published29 June 2019

- Published14 May 2018

- Published7 March 2019

- Published30 November 2018

- Published16 April 2019

- Published5 April 2019