Mental health: Trauma, genocide and my invisible illness
- Published
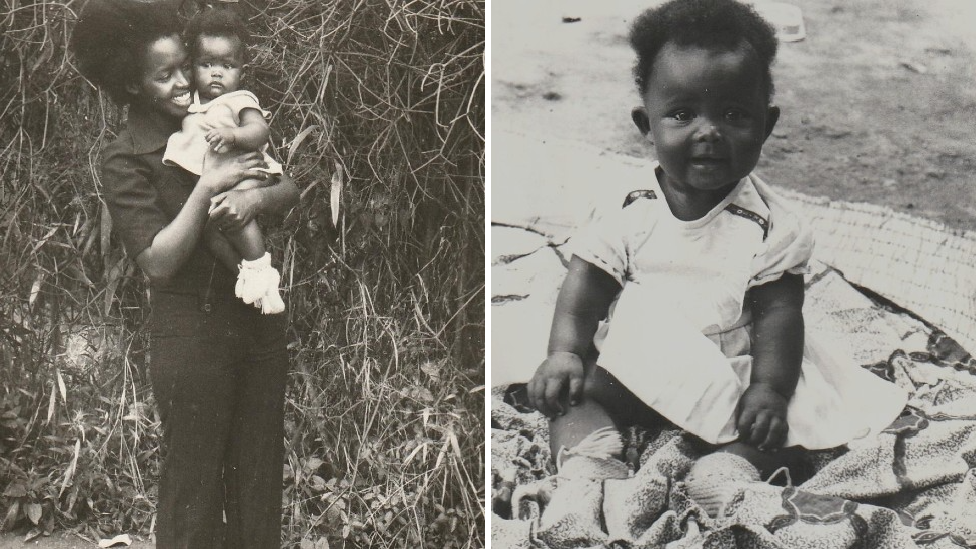
Victoria was born in Rwanda in 1981 and grew up in the capital, Kigali
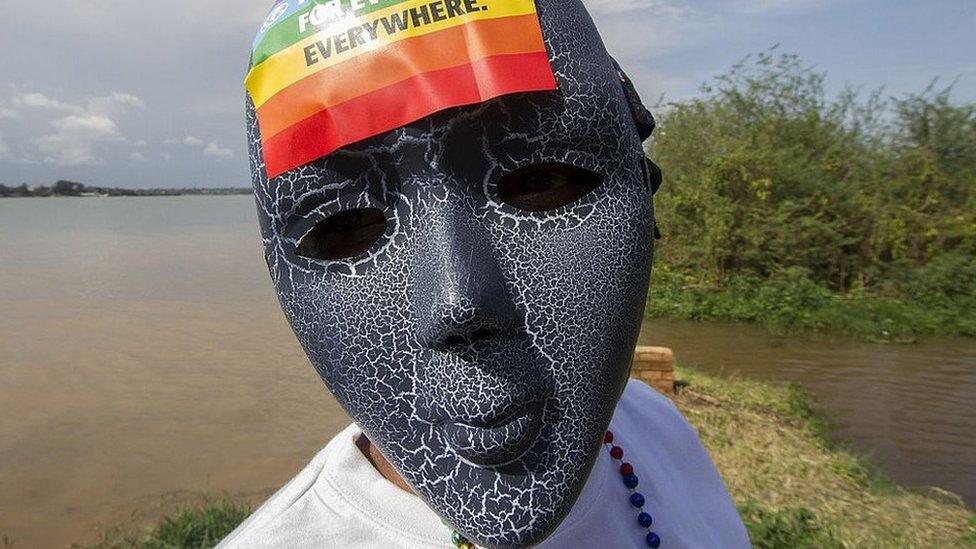
I have an invisible health condition that is not often talked about.
This is the first time that I am describing my issue, which is deeply personal and has remained hidden from many of my friends and colleagues for years.
But the truth is that for much of my life I did not know that I had the condition or what it was called.
Now I recognise that after having lived through the genocide as a child growing up in Rwanda as well as other troubling events, I have post-traumatic stress disorder, also known as PTSD.
It triggers panic attacks that can come at any time and which leave me struggling to breathe. I am usually covered in a thin layer of cold sweat when they subside, as I fight to get back to my "normal" self.
Looking back, I was your regular happy child, growing up in the 1980s initially in a small but supportive family in Rwanda's capital, Kigali.
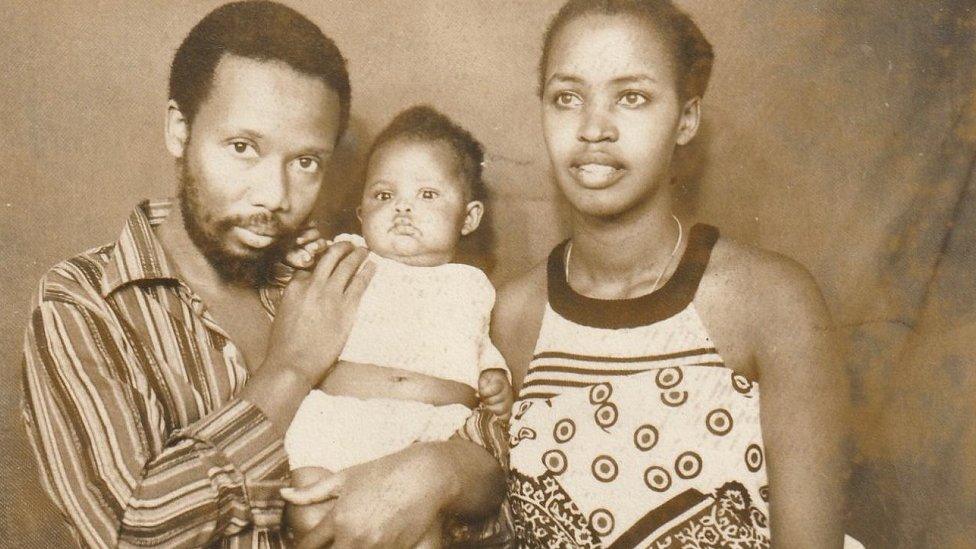
Victoria was brought up by her mother but is pictured here with both her parents
Essentially, it was myself, my mother and my little brother, Junior.
But this little angel would not live to see his first birthday, and his death, when I was around the age of two, from a severe coughing illness would be my first real sense of loss.
I could not comprehend the emptiness I felt, because I was a child myself, but over time I have come to see this as the possible start of my journey, the genesis of my PTSD.
The second gut-wrenching event came when I lost my mother to illness, two months before I turned 10.
I can still remember being in bed with her in the hospital, wanting to be close to her because I loved the way she smelt of sunshine. But when I touched her skin it was very dry. It was like there was nothing left of her as she had lost so much weight.
After she died, my world as I had known it up to that point was over, but I did not grieve as I just had to get on with things. I moved in with my aunt - who I now call my mum - and five cousins, all of whom were very supportive.
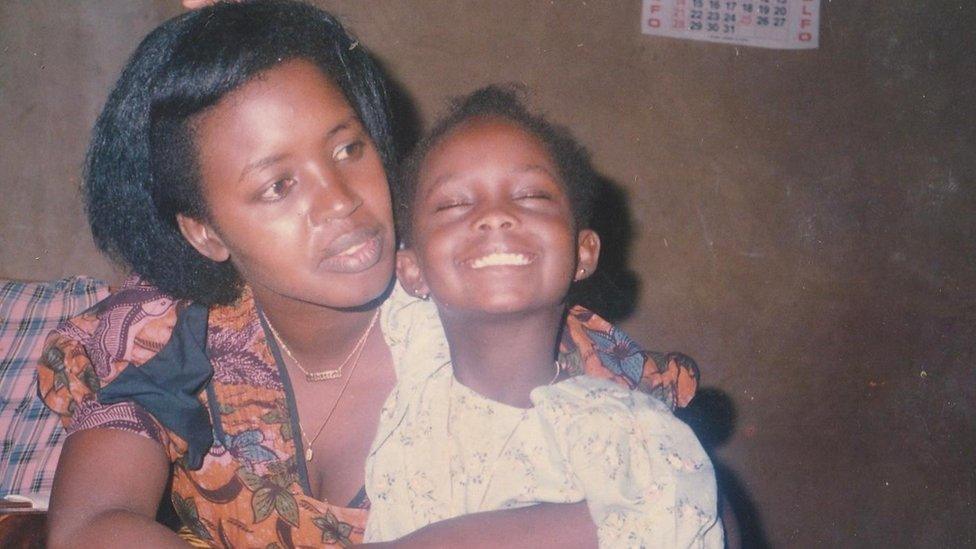
Victoria was nine when her mother, pictured here, died and she moved in with an aunt and her family
Then, in April 1994, when I was 12, my life was completely upended by the genocide.
In just 100 days, 800,000 people would be killed by ethnic Hutu extremists targeting members of the minority Tutsi community, as well as their political opponents, irrespective of their ethnic origin.
To the sound of gunfire we fled Kigali for Gisenyi, a town close to the border with the Democratic Republic of Congo.
But the violence followed us and while travelling in the area around Gisenyi we were often stopped at roadblocks by militia fighters. One time they grabbed my little sister Nelly but my mum somehow talked them down from killing her.
That was a scary moment, when I realised that these people - who looked drunk and out of their minds - could do anything to us.
Some were quite young, but they had machetes, they had wooden clubs and some of them had blood on them.
This is something that will stay with me forever.

More on the genocide in Rwanda

We then crossed the border and became refugees in the Congolese town of Goma. I witnessed more death there as people were dying of cholera and dysentery and the bodies were piling up on the side of the road.
Throughout this time and then our move to Kenya and finally, when I was 16, to Norway, where we were resettled, I was in survival mode.
This is a psychological state that allows people to deal with stress, but if you live with it for too long it can be damaging.
However, once in Norway, when I began to feel more relaxed, the panic attacks began and a psychologist identified that I was suffering from PTSD.
Of course, I am not alone.
More than one in five people who have lived through war in the last decade are thought to have some type of mental health condition, including PTSD, the World Health Organization found.
And the condition can be the result of many different kinds of traumatic event.
According to the Public Library of Science medical journal, people living in sub-Saharan Africa are disproportionately exposed to trauma and may be at increased risk of PTSD.
But in many countries, mental health care and help is often either lacking or very limited.
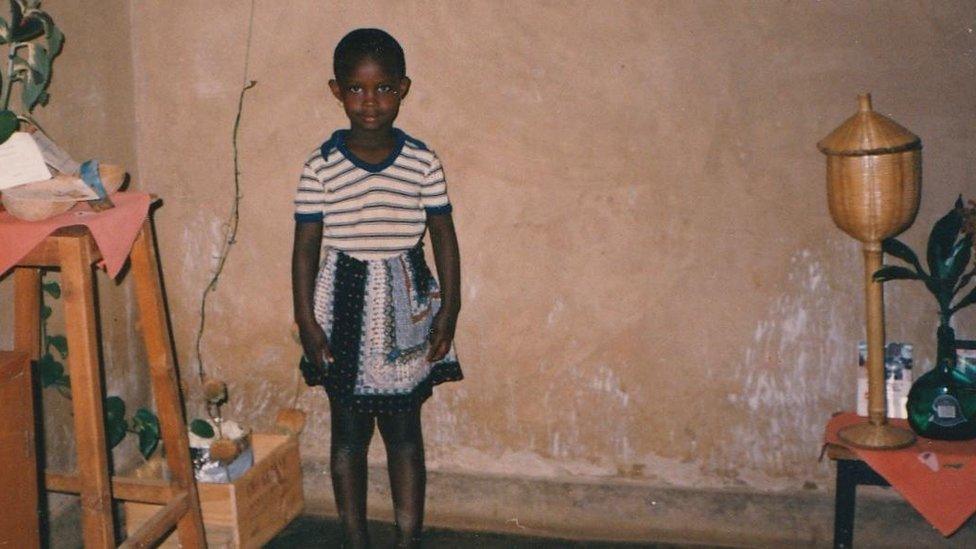
Victoria understood later in her life that her trauma began at a young age
Take for example Sierra Leone, which has been through so much - a decade-long civil war, natural disasters that killed hundreds and an Ebola outbreak in 2015 that left almost 4,000 people dead.
The WHO estimates that 10% of the country's seven million population have mental health problems but only a tiny percentage are able to access mental health services.
"[When the war ended] there was a lot of talk about reconciliation, and peace-building," said Dr Rebecca Esliker, a clinical psychologist at the University of Makeni, in the country's northern province.
"But we didn't address the mental states many people had, the traumatic events that people went through, and those atrocities people experienced, and what remains in their minds."
Speaking to BBC podcast The Comb, Dr Esliker added that soon after the war, NGOs and other international organisations went to Sierra Leone and did two or three weeks work of what she calls "crash courses" to train people in counselling.
She argued that this would not have been enough to help Sierra Leoneans deal with the trauma they had gone through and as a result, the country continues to bear the consequences of all the untreated traumas, even to this day.
"We are seeing people who are trying to cope, especially those who were young during the war. We are seeing a lot of people dealing with serious mental disorders, which sometimes lead to a lot of aggression, fighting and domestic violence."
I am one of the fortunate ones to have lived in countries where mental health care is easily accessible"

When I hear this I think myself lucky.
I have not exhibited the symptoms in the way that Dr Esliker describes, but I know many who do.
I am also one of the fortunate ones to have lived in countries where mental health care can be easily accessible and sometimes does not cost much.
But even in most developed countries, there remains widespread stigma about mental health conditions.
In a 2015 study in the UK, nearly nine out of 10 people with mental health problems said the stigma they experienced had a negative impact on their lives.
This often leads to people living with mental illness to shy away from seeking the help they need. We must simply stop calling people with mental health conditions "crazy".
It has taken me over 30 years to loudly and openly say that I have PTSD, and if I had not told you, you would not have known.
It is important to talk about these things with honesty and without feeling shame. Then maybe more people will seek the help they need.
Related topics
- Published15 June 2020

- Published19 June 2019

- Published23 September 2019
- Published20 April 2021