African Covid patients 'dying from lack of oxygen'
- Published

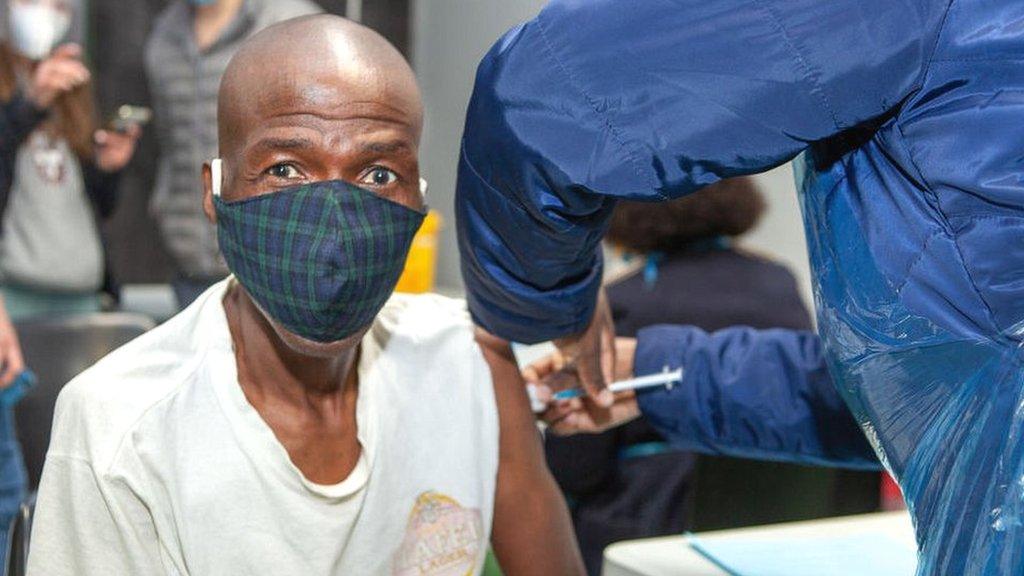
"It is really stressful to work in this condition," says Dr Mahamud whose patients are dying because of a lack of oxygen
Many African countries are facing a "growing crisis" of severe oxygen shortages which is leading to preventable deaths, international health agencies have warned.
A doctor in Somalia's semi-autonomous region of Puntland told the BBC that between five and 10 of his Covid patients were dying because of a lack of oxygen almost every day.
"These would all be preventable deaths if we had adequate oxygen," said Dr Jama Abdi Mahamud at the government-run Gardo General Hospital.
There are no official figures available showing a rise in preventable deaths, but many low-income countries are struggling to access oxygen supplies amid surging coronavirus cases, and limited or no access to coronavirus vaccines.
Every Breath Counts, a coalition of global health campaigners, say 18 low-income countries are currently dealing with oxygen shortages or are at risk of facing the crisis, with most of those being in Africa.
"The G20 Global Health Summit leaders didn't mention oxygen at their meeting in May, but the G7 has now signalled there will be financial support for oxygen," said Leith Greenslade, co-ordinator of the coalition.

Most of the lowest countries dealing with oxygen shortages or at risk of facing the crisis are said to be in Africa
Jessica Winn, head of pneumonia support hub for Save the Children, said the need for oxygen in these countries was high and urgent.
"Now that a third wave of the pandemic has arrived in Africa, populations are again at risk. Since 1 June 2021, the oxygen needed to treat Covid-19 patients in Zambia has increased five-fold to 50,000 cubic meters, and three-fold to 12,000 cubic meters in the Democratic Republic of Congo.
"Demand for oxygen to treat Covid-19 patients is steeply rising in Zimbabwe."
A study published in the Lancet last month suggested more than half of the Covid patients that died in 64 hospitals in 10 African countries were not given oxygen.
'No oxygen plants'
Dr Mahamud said that during the second wave in Somalia up to 25 people were dying each day in his hospital because of a lack of oxygen: "It is really stressful to work in this condition."
According to World Health Organization (WHO), of the 14,823 confirmed coronavirus cases in Somalia as of 16 June, 775 people have died.
Health professionals say the real figure could be many times higher because there is no proper reporting mechanism, and many deaths occur in villages.
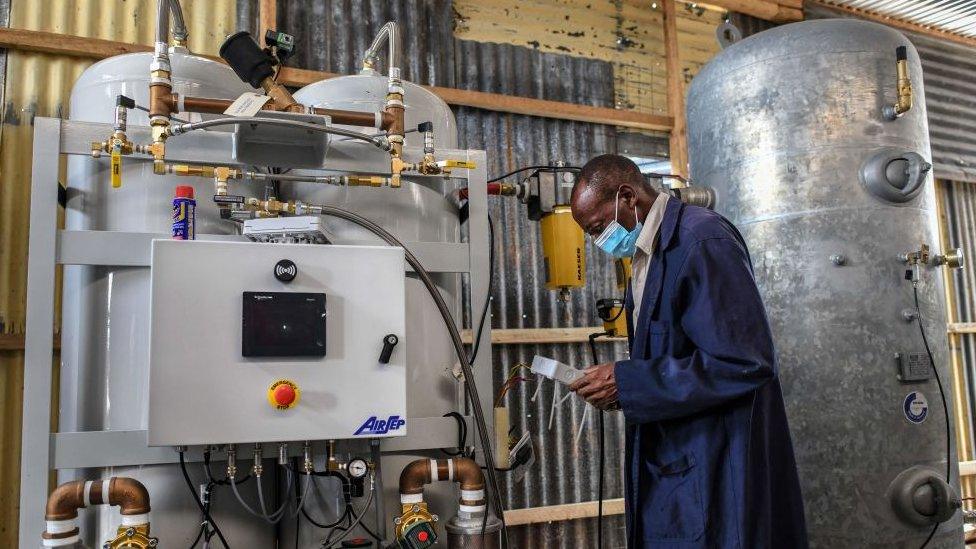
Oxygen plants in the few hospitals that have them are said to break down frequently because of the increase in production
"There are around 750 hospitals and primary health centres across Somalia which urgently need more than 1,400 oxygen concentrators, but they have received less than 300," said Dr Joseph Serike, senior health technical specialist with the Save the Children in the capital, Mogadishu.
Government officials admit it is a growing challenge.
"No government-run hospitals have oxygen plants. Only three private hospitals in the capital, Mogadishu, have them," said Dr Ubah Farah Ahmed, director of family health department at Somalia's health ministry.

You may also be interested in:
Fake news and mistrust in the government mean a lot of Nigeria's population thinks the pandemic is a hoax.

In neighbouring Ethiopia, health officials said some government hospitals had oxygen plants but they are overwhelmed because they now need to supply to other hospitals too.
"And because of the high production pressure, the plants break down worsening the shortage," said Dr Menbeu Sultan, chair of Ethiopian Society of Emergency Medicine Professionals.
"The shortage is severe in remote and very poor places because they have no production of their own.
"And lorries carrying oxygen cylinder have to travel hundreds of kilometres to reach such places and in some cases it is too late for patients who urgently need the gas."
As of 16 June, Ethiopia has seen 274,346 confirmed Covid cases and 4,250 deaths.
During the last major wave between April and May, Ethiopia needed around 15,000 cylinders of oxygen in a day, according to an oxygen-need tracker updated by Path, an international non-government organisation working in health sector.
It shows the need is now down to 1,200 cylinders per day but experts with the tracker said their calculation is based on reported Covid cases and most of the cases in the country go unreported.
In DR Congo, the demand has gone up to nearly 2,000 cylinders per day from less than 500 earlier this month, according to the tracker.
'Blind spot'
Experts say many of the lowest-income countries in Africa, like very poor countries elsewhere, lack commercial oxygen production facilities, which could then potentially divert supplies to hospitals to help during emergencies.

Providing high-flow oxygen, critical for Covid-patients, can be a problem
As a result, very few hospitals can supply high-flow oxygen that critical Covid patients need, health experts say.
"In our whole country, only one hospital has the capacity to treat at a time more than 10 patients needing high-flow oxygen and their Covid unit is usually full," said Dr Sarah Wandia, who works in Maua Methodist hospital in Kenya.
"We lost two patients from our hospital waiting for the space in that unit.
"Our hospital's current oxygen plant has the capacity of producing 45 litres of oxygen while one Covid patient can use 15 litres of oxygen leaving a precarious amount to care for premature babies, intubated patients in the operation theatre and in the accident and emergency department."
Health experts say it took a year for oxygen supply to be recognised as an essential medicine in the global strategy to treat Covid patients.
"The impending crisis was a blind spot for the global health community for a year," said Ms Greenslade of Every Breath Counts.
International financing agencies like the Global Fund say they have now made fast-track funding for oxygen available to some lowest income countries including The Gambia, Kenya, Malawi and Tanzania in Africa.
"With the help of donor agencies, we will soon install 10 oxygen plants in some government hospitals," said Somalia's Dr Ahmed.
Related topics
- Published31 December 2021