India Covid-19: Bihar braces for 'coronavirus storm'
- Published

Bihar has ramped up coronavirus testing but it's still too low, say experts
When Gopal Singh complained of severe chest pain on 18 July, his family got worried.
The 65-year-old had a history of breathing illnesses, and he had also suffered a heart attack in 2013.
So he got tested for coronavirus immediately. The result was positive.
His family rushed him to the government hospital in their home town of Katihar in the northern state of Bihar. The doctor advised them to take him home, which surprised his son, Vishal.
He told the doctor that his father had recovered from severe pneumonia last year, and was at higher risk. But the advice remained unchanged.
Even as the family arranged an oxygen cylinder at home, Vishal began contacting other hospitals. None had beds available.
Over the next 24 hours - as Mr Singh's blood oxygen level kept falling - Vishal got through to a government hospital that had an ICU bed free.

Vishal (left) with his mother, and father Gopal Singh
But it was 90km (55 miles) away and he had to find an ambulance to take his father there, which he did.
They were on the way, and nearly at their destination, when it ran out of oxygen. Vishal frantically called the hospital and asked for an oxygen cylinder to be made available at the gate.
When they finally arrived, there was no-one at the gate - and they were told there were no ICU beds available. They were asked to take Gopal to the isolation ward.
It was on the third floor and the lift wasn't working. So Vishal and his 60-year-old mother took his father up the stairs on a stretcher. Vishal says no doctors or nurses came to see Gopal.

In some cases, family members of patients have had to buy oxygen cylinders
He found 10 oxygen cylinders outside the ward, but none were full. He says he used them, switching the cylinders again and again through the night.
By the morning, they decided to shift Mr Singh to another hospital. They had barely driven for an hour when he died.
"I did everything to save him but the system defeated us. He didn't die, it's murder. He kept asking me to save him - he was so scared," Vishal says.
"I will never forget his pleading eyes."
Mr Singh's death is proof of the grave challenges that face Bihar, one of India's most populous and poorest states, in its fight against Covid-19.
'We didn't plan on the right scale'
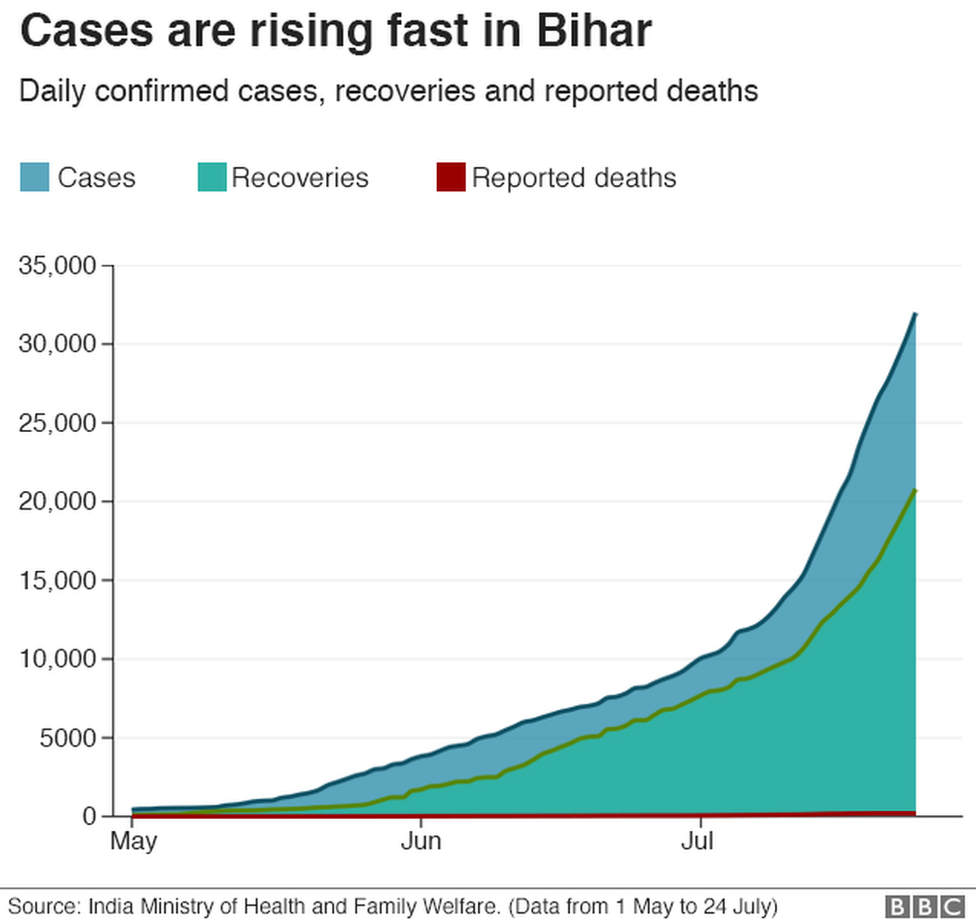
So far, Bihar has recorded more than 33,000 cases, most of which were added in July. But it has reported relatively few deaths from the virus - 217. That's a far lower death-toll than that of Andhra Pradesh (884), another state which is witnessing a sharp uptick in case numbers.
But that could change quickly, say doctors and experts, because the state did not do enough to shore up its crumbling health infrastructure in time.
More than 40% of the posts for healthcare workers are still vacant, says Dr Sunil Kumar, the secretary of the Indian Medical Association (IMA) in Bihar. This is despite repeated requests to the government, he adds.
"We knew Covid-19 will strike the state sooner than later, but we did not plan at the scale we had to," he says.

Most districts in Bihar also don't have enough ventilators, which have become crucial in treating emergency Covid-19 cases.
"There is an acute shortage of doctors who are experts in operating the ventilator - this is a very specific requirement - and the state should have thought about it," Dr Kumar says.
The state government denies lapses on its part, and has said it is building additional health infrastructure rapidly.
But Bihar faces unique challenges: For one, its primary healthcare network is weak and suffers from decades of neglect. Many states have used those networks to test and trace effectively, or create awareness about hand-washing and wearing masks.
It also has fewer top-rung government hospitals or private ones, which can accommodate and treat patients swiftly. While big cities such as Delhi and Mumbai have also seen deaths due to delayed admissions, experts fear that similar pressure in Bihar could lead to a far higher death toll.
To make matters worse, flooding has begun in several parts of the state, further stymying its response.
'Virus is going unchecked'
Dr Kumar says the rise in case numbers shows that the infection is spreading fast, and to remote corners of the state.
While Bihar has ramped up testing, its testing rates are still among the lowest in the country.
That becomes clear when you compare Bihar's tests per million - about 3,500 - to Andhra Pradesh's figure - some 28,000. Uttar Pradesh, a state more comparable to Bihar in terms of resources and population size, is doing more than 7,000 tests per million.
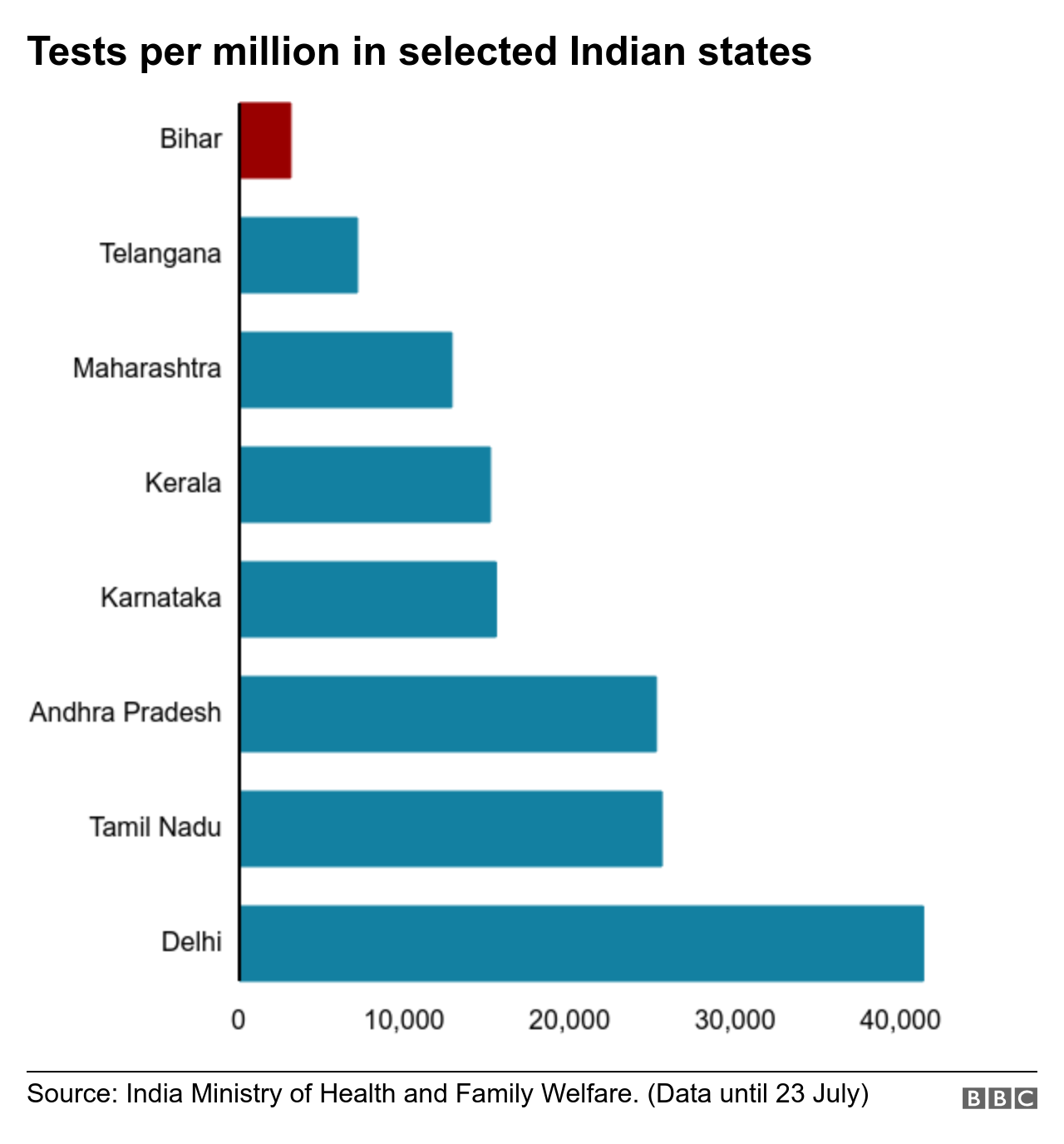

Bihar is now averaging about 10,000 tests a day, but that's still too little considering it's home to more than 100 million people, Dr Kumar says.
"This means that many infected people are going unchecked and spreading the virus into communities," he adds.
Bihar had the benefit of learning from states like Delhi, Maharashtra and Tamil Nadu, where the infection raged in May and June. And a stringent nationwide lockdown - through April and May - also gave officials the opportunity to prepare for a rise in case numbers.

PPE kits were discarded just outside some hospitals in Bihar
But they didn't act swiftly, failing to increase testing. And the caseload too remained among the lowest in the country until June.
The situation began to change when the lockdown forced migrant labourers, suddenly out of work and money, to return home to Bihar.
A doctor, who did not wish to be identified, said there were glaring lapses in testing and quarantining the workers who came home.
There were reports of people running away from quarantine centres because of bad management, and some completely dodging the screening process.
"All those lapses are now costing the state - people are dying because of that negligence," the doctor says.
'It's looking grim'
Timely testing and the quality of treatment continue to be a challenge.
Rajnish Bharti had a high fever and cough when he went to the government hospital in Bhagalpur district on 9 July.
He was told to come back 10 days later as "there are too many people on the waiting list".
Mr Bharti's condition worsened in that time, and he was admitted to the hospital as soon as he tested positive for the virus.
He says he met a doctor the day he was admitted, but no-one has visited him in the week since.

Several patients had to be given oxygen in hospital waiting areas
"A ward boy (helper) comes and throws medicines in the room. It's been happening for five days," he says.
He adds that he is worried he may not get oxygen in time if his condition deteriorates.
There is a phone number that patients can call in case of an emergency, but it's not manned 24x7.
But those with "connections" can get treated quickly, Mr Bharti says. By that he means those who are wealthy or powerful enough to pull strings.
"If some VIP calls on your behalf, you are immediately looked after," he adds.
A senior journalist in Patna, the state's capital, who also did not wish to be named, said this was not unusual. "Connections matter in states like Bihar, and that often leaves out the poor who have nowhere to go," he says.
"But the way caseload is going up, I doubt that even connections will be of any help in the future."
A government doctor in Gaya district says the pressure on the system is already building up.

Staff shortages mean family members often help patients, and without protective gear
"There is an acute shortage of staff, and I end up looking after 50-80 patients alone, with just a nurse to help," he says.
He says that at times, there aren't enough cleaning staff or assistants because they are all employed as contract workers with poor pay and no protection.
"They don't listen to us and I can't blame them. Would you bet your life for 5,000 rupees ($66: £52) a month? That's just peanuts," he adds.
"We doctors are doing what we can, but I am really worried. It's looking more and more grim every day as I see people struggling to save their loved ones."
Data analysis and charts by Shadab Nazmi
- Published21 July 2020
- Published17 July 2020
