Bipolar disorder: The group changing attitudes about the condition
- Published
Data shows that at least 0.3% of India's population lives with bipolar disorder (file picture)
Living with bipolar disorder is not easy. Many people do not understand the condition and patients suffer discrimination as a result. An online community in India is now trying to change such attitudes, writes Urvashi Sarkar.
Vijay Nallawala was 40 when his family noticed that something was not quite right with him.
"I would suddenly be euphoric. And then I would abruptly plunge into depression, getting up in the wee hours of the night and writing extremely dismal poetry. The swings were very abrupt," he says.
This wasn't the first time though - Mr Nallawala says he first started to experience such symptoms when he was 14. "But nobody quite knew what was the problem, except that something was amiss."
This time he sought medical help. In 2003, he was diagnosed with bipolar disorder - a condition that makes people go through extreme mood swings. People can suffer episodes of depression - which make them feel very low or lethargic - or mania - where they feel high and overactive.
Mr Nallawala, now 60, has been stable for the "last five or six years", he says. But his struggles made him realise the need to create awareness about the condition.
In 2012, he began blogging about it. A friend then encouraged him to set up Bipolar India, a website which creates awareness about the disorder, collates mental health resources and gives others with the condition a platform to share their experiences. Today it has over 500 members.
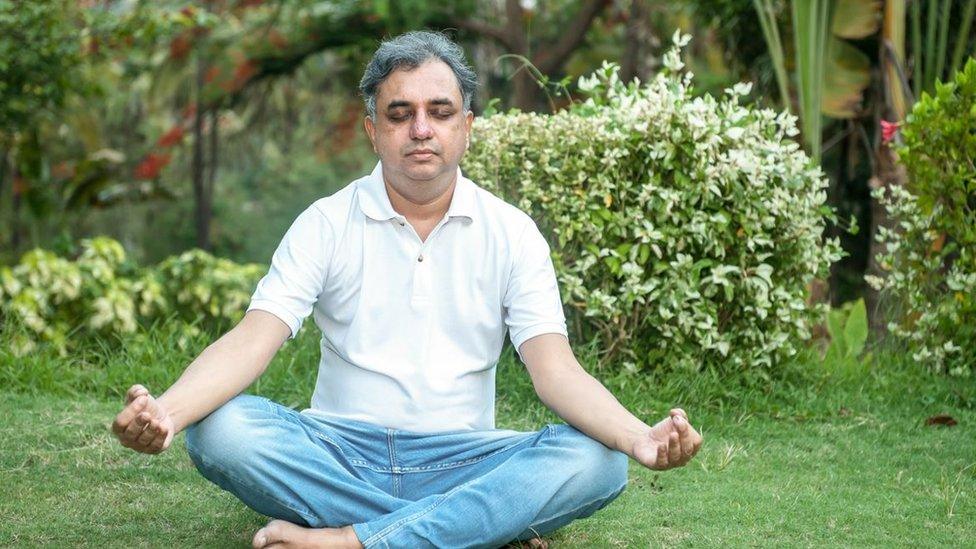
Vijay Nallawala launched Bipolar India in 2013
At least 0.3% of Indians live with bipolar disorder, data from India's National Mental Health Survey 2016 shows. But stigma and lack of awareness around it continue to have a devastating impact on the lives of patients who routinely face discrimination.
A dearth of qualified professionals - India has just 0.75 psychiatrists per 100,000 people - makes matters worse.
Nine years after he set up Bipolar India, Mr Nallawala spends a chunk of his day checking messages on the community's main Telegram group. It has members from all big cities including Mumbai, Delhi, Bengaluru, and Chennai and regularly organises in-person meets.
Mr Nallawala says he wanted to build a sense of community and offer emotional and sometimes financial support to those living with the condition.
"Our community could actively avert four suicide situations though we aren't trained as suicide gatekeepers. In one instance, we managed to raise funds for someone who needed urgent hospitalisation," he says.
Patients often suffer because of the lack of access to healthcare. India's laws make it mandatory for insurance companies to provide coverage for mental illnesses. But firms rarely do that, Mr Nallawala says.
Bipolar India has tried to bridge the gap. The group has launched a programme which connects its members to organisations that are willing to offer them jobs.
"We firmly believe that recovery from mental illness is incomplete without rehabilitation," Mr Nallawala says.

People with bipolar disorder suffer episodes of depression when they feel very low and lethargic (file picture)
The group has helped people such as Tripti Mishra, 57, who had to see 13 doctors before she found someone who could explain the disorder to her.
"I don't think [the earlier doctors] were really listening. I wanted to know what was happening to me and why it was happening," says Ms Mishra, who lives in Durgapur city in West Bengal state.
A retired professor of computer science, Ms Mishra still considers herself lucky - she says she had an extremely supportive family.
She says that joining Bipolar India changed her life. "I realised I am not alone and this is a powerful feeling. I could talk to other people, discuss coping strategies, and share mutual fears, guilt, and insecurities," she says. "In families, these feelings may not be completely accepted or acknowledged."
The group is also open for caregivers to join.
Mumbai-based Venkateshprasad Narayan Iyer and his wife are caregivers to their 31-year-old daughter who is bipolar with schizoaffective disorder, external. They joined BipolarIndia because they felt that they "have to take care" of themselves.
"We realised that apart from dealing with the emotional, spiritual and financial crisis of your child, we have to take care of ourselves. The caregiver also falls into depression but needs to have continued love and compassion for their child and also a zest for living," Mr Iyer says.

Venkateshprasad Narayan Iyer is a caregiver to his 31-year-old daughter
But this is hardly easy in the absence of reliable, affordable institutional facilities to help take care of patients, especially when they are experiencing particularly low phases.
This means that there is no respite for caregivers, who also worry about the future of the people they love.
Debashish Ghosh and his wife Supriya (names changed), based in Gurgaon city, have been full-time caregivers for 15 years to their 38-year-old daughter who has schizophrenia. But they still find it hard to come to terms with their daughter being "a little different from others".
"She desires a career, marriage and child but her fluctuating moods prevent her from stability. She cannot earn despite wanting to. Who will take care of her after us?" Mr Ghosh asks.
The couple say that ever since their daughter was diagnosed, they have avoided meeting friends and families, afraid they would judge her.
Experts say people with mental illnesses are stigmatised because references to bipolar disorder and schizophrenia are still rare in India.
"There is more openness and acceptability about depression than before. But depression is spoken about in a generic sense and people may not really understand the illness being discussed," says Dr Milan Balakrishnan, a consultant psychiatrist and former secretary of Bombay Psychiatric Society.
Dr Balakrishnan says initiatives like Bipolar India can go a long way in changing such attitudes.
"Such groups have a powerful impact because they provide support and checks in different situations, say if medication is stopped, or if people are experimenting with substances that can trigger relapses. Caregivers burn out very fast," he says.
"The group offers a beacon of hope for these communities."
Related topics
- Published16 October 2018

- Published16 December 2021

- Published31 October 2021
