Coronavirus: What does a working 'test and trace' system look like?
- Published

Guernsey has not found a new Covid-19 case since late April, thanks in part to its "test, trace and isolate" system
Health Secretary Matt Hancock has expressed "renewed confidence" NHS Test and Trace will become the "world-class system" promised by the prime minister - although Mr Hancock acknowledged the system needed to get "better and better" as it developed. But what does an already world-beating test and trace programme look like?
There is no need to look as far as Singapore, South Korea or even Germany for one; an extremely successful example can be found much closer to home.
Guernsey has not recorded a new coronavirus case since 30 April and there are no active Covid-19 patients in the island.
This has led to significant easing of its lockdown rules and the Channel Island's 63,000 residents can go shopping, get a haircut and meet up with friends and family.
Such is the success of the response, from 20 June the government will remove nearly all lockdown restrictions and life will effectively return to normal, with no social distancing requirements for businesses or restrictions on gatherings.
Overall, 252 people in Guernsey are recorded as having contracted coronavirus between 9 March and 1 May, with 13 people confirmed to have died with the virus and three further suspected Covid deaths.

Pubs are open, but people must leave their contact details with the business if tracing them becomes necessary
The people of Guernsey are currently the only ones in the British Isles who can lawfully drink a pint in a pub without a meal - landlords aside.
Currently, everyone who enters a "controlled environment", like a pub, restaurant or hairdressers, must leave their name and contact details with the business.
These must be available at all times for the island's Public Health Services to access, should a new case be found, however this restriction will also soon be lifted.
It's an imposition that does not seem to trouble people enjoying a drink in the sunshine at the Rockmount in Cobo.
One of them, Colin Saxby, said the ability to order a pint was "very pleasant", especially when the weather was good.
"I like a beer and crossword at lunchtime, so I'm quite happy."

Guernsey is the first place in Britain to let people have a drink without a meal
According to the island's director of public health, Dr Nicola Brink, the backbone of this relaxation of lockdown was the early and rigorous implementation of a "test, trace and isolate" system.
Dr Brink said she began preparing at the end of January, by which point it had become "clear" to her Covid-19 had "pandemic potential".
With just one hospital and a relatively elderly population - nearly 20% of islanders are over 65 - a serious outbreak could have been catastrophic.
The trained virologist's calm presence at live-streamed government briefings has turned her into something of a local celebrity.

Dr Nicola Brink has put herself front and centre in keeping the public informed
She began recruiting contact tracers in January and by the time the first confirmed case was found, they were "ready and waiting".
Dr Brink said: "Having those trained individuals on the 9th of March meant we were able to implement our programme immediately."
So far, contact tracers have spoken to 1,757 people in the island - the equivalent of about 1.8 million in the UK.
However, despite this early action, the response was not without challenges.
During the height of the crisis in mid-March, when cases were emerging rapidly and there were concerns the health service could become overwhelmed, the speed of returning test results became a significant problem.
Guernsey was entirely dependent on UK laboratories and was unable to "deliver our strategy efficiently", Dr Brink explained.
She said: "We were waiting two or three days for a test result and that was not enabling us to respond."
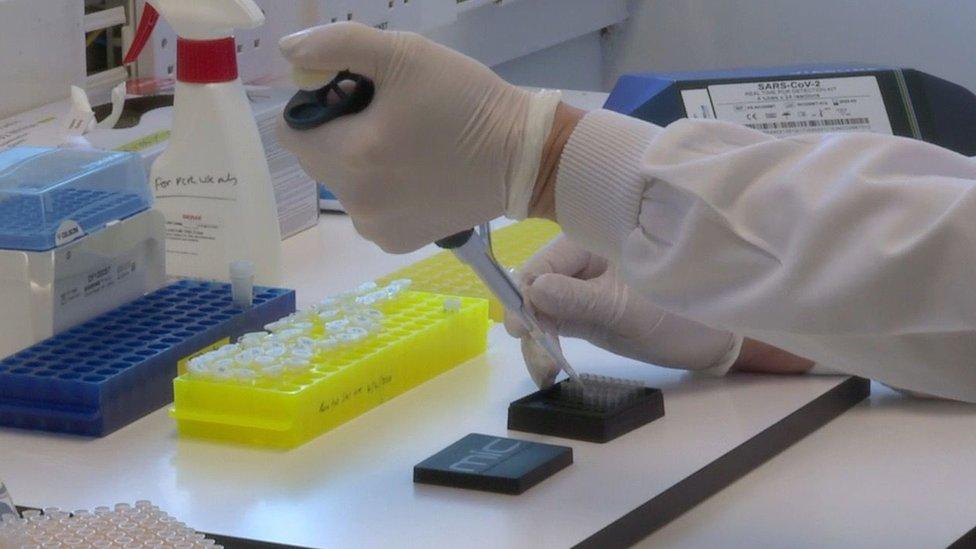
Guernsey set up its own testing capacity when it became clear relying on the UK could hamper the ability to control the spread of the virus
As a result, schools were closed on 22 March and a full lockdown was introduced three days after.
Fortunately, the Public Health team realised delays were a possibility and had already ordered the equipment needed to set up on-island testing at the beginning of March.
The project came together with "remarkable" speed, and the capacity to test an equivalent of 160,000 people daily in UK terms was up and running by the end of the month, Dr Brink said.
This will have increased to 400,000 by July, once an expected shipment of testing equipment arrives and is installed.

Dr Brink has become a recognisable figure in Guernsey by appearing on live streamed government briefings
Because Guernsey is a Crown Dependency, it has total control over its borders. A mandatory two-week quarantine for new arrivals was imposed on 19 March, which will remain in place even after life returns to near normality to prevent reintroducing the virus.
This ability to regulate who comes in and goes out of the Bailiwick, which also includes the islands of Alderney and Sark, has been fundamental to its response to the pandemic.
Dr Brink herself acknowledges the advantageous position, and how test and trace is "ideal" for the island.
A difficulty the team encountered as the pandemic progressed into April was over concerns they were not picking up on symptoms.
Dr Brink said a review of their own cases and the evidence coming from around the world led them to expand their list of symptoms early on.
By 8 April, they had included the loss of smell and taste to their list which would cause people to get tested, nearly a month before the UK did so.

The Bailiwick locked down on 25 March
Guernsey's contact tracing system is based around interviewing coronavirus patients over the phone and establishing who could be at risk.
An essential part of this process is establishing a "rapport" with them and building trust, Dr Brink said.
She said: "It's really important that we provide people with detailed explanations of what we're doing.
"They're entitled to that information and if people have it they are more likely to co-operate and understand."
Nurse Andrea Tostevin was trained as a contact tracer in January. She said it was essential people doing the work had good communication skills.
Case interviews, where contact tracers establish who patients have interacted with, begin within an hour of the test results coming in, Mrs Tostevin explained.
She said: "Some people are quite unwell and worried about themselves and their family.
"It's important you could give some reassurance and have the information."

Andrea Tostevin said most people she spoke to had been supportive of their efforts to trace and isolate potential cases
Mrs Tostevin explained that a small number of those being asked to isolate for two weeks were confused or pushed back at her, but the vast majority were happy to comply with the restrictions.
"People who were several days from their contact and feeling really well would occasionally question 'why do I need to do this?'."
However, she said they were invariably able to explain the public health rationale for self-isolation and get sceptical people on board, praising the "community spirit" shown by most people.
Dr Brink echoed this view, praising the "incredible support" of the people of Guernsey for their response to the pandemic.
She said: "It's been incredibly humbling. At times, at the end of a long day, it's the type of thing that's kept me going."

A SIMPLE GUIDE: What are the symptoms?
RISK AT WORK: How exposed is your job?
HOW A VIRUS SPREADS: An explanation
RECOVERY: How long does it take to get better?

- Published11 June 2020

- Published11 June 2020
- Published11 June 2020

- Published5 August 2021

- Published3 June 2020

- Published27 May 2020
