Acclaimed scientist gets brain surgery for alcohol addiction
- Published
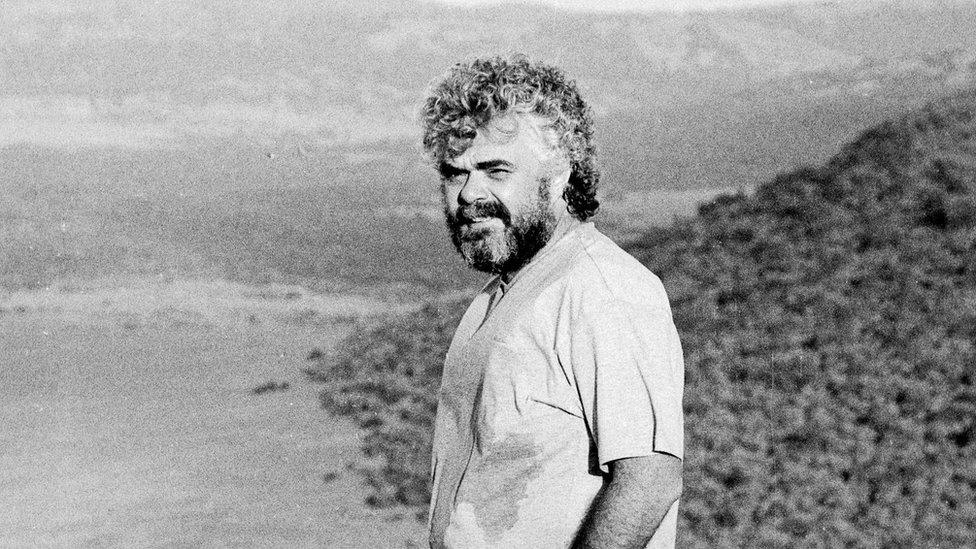
Microbiologist Frank Plummer is recognised globally for his research into the HIV virus
Microbiologist Frank Plummer has been on the frontlines of the battle against of some of the world's most alarming epidemics, from HIV to Ebola - but his illustrious career masked a growing reliance on alcohol. Now, the researcher has become the guinea pig in a clinical trial investigating whether brain implants can help treat alcohol use disorder.
Alcohol was always a big part of Frank Plummer's life.
At the beginning of his research career, in the early 1980s in Nairobi, he began to lean on scotch to relax, and to the handle stress, disappointment and grief related to his work.
He and his colleagues were feeling the visceral urgency of their work as they watched the African HIV crisis unfold.
"I felt just like a fire fighter or something but the fire didn't go out," Dr Plummer, 67, told the BBC.
"It just kept going and going and going. There was this sense that you needed to do something and that the world needed to do something. And I was trying to draw attention to it and get money to continue our work. So it was a time of intense pressure."
Dr Plummer's research subjects were Kenyan women, sex workers, some who were found to have a natural immunity to the virus.
It was pioneering research, and over the 17 years Dr Plummer spent in Kenya, he and his colleagues made groundbreaking discoveries made about how HIV spreads - breakthroughs that have helped inform how we reduce transmission risk and that raised the possibility a vaccine against the virus could be developed one day.
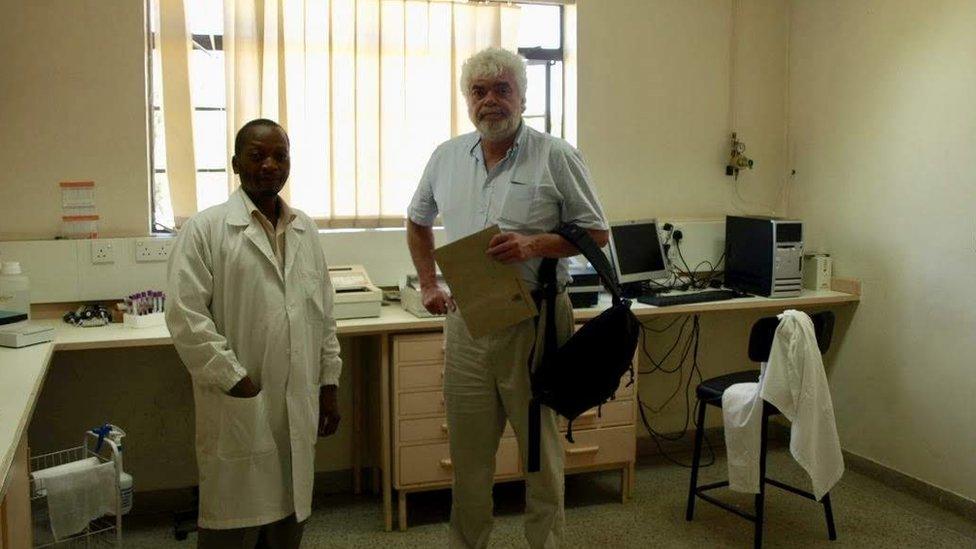
The University of Manitoba and the University of Nairobi have long collaborated on HIV research
In those stressful times, five or six glasses of scotch a night were giving him room to exhale after hectic days and weeks.
When he returned to Canada, he took a leadership position at Winnipeg's National Microbiology Laboratory, one of a handful of laboratories in the world with the capacity to work with highly pathogenic viruses like Ebola.
At the lab they dealt with the outbreaks of Sars in 2003 and the H1N1 influenza in 2009. It was there Dr Plummer contributed to the development of Canada's Ebola vaccine.
It was vital, exciting, and stressful work, with 12-hour days that began with coffee and would end with several glasses of scotch. His drinking escalated to about 20 ounces of the booze a night.
It didn't seem to affect his work - until 2012, when it caught up with him.
"My liver packed it in," he says. "Before that I knew I drank a lot but I didn't think I had a problem."
The diagnosis of chronic liver failure was followed by a liver transplant. He had to watch his alcohol intake to preserve his new liver - but he found his alcohol had become a powerful thirst.

Frank Plummer found he was drinking multiple glasses of scotch a night
Dr Plummer tried treatment - rehab programmes, support groups, counselling, medications - but any relief was temporary. He would inevitably slip back into drinking.
"It was pretty hopeless cycle and it was very tough on my family and my wife, Jo, and on my children and my stepchildren," he says. "I was in the hospital a lot, I almost died several times."
He went looking for help - "a more robust clinical solution, perhaps one not yet discovered" - and was referred to two neurosurgeons at Toronto's Sunnybrook Hospital.
They were recruiting patients for an experimental procedure being conducted in North America for the first time, using deep brain stimulation (DBS) to help patients with treatment-resistant alcohol use disorder. The surgical trial is testing how safe and effective DBS is for alcohol addiction.
DBS has been used for over 25 years to help treat movement disorders like Parkinson's disease. Roughly 200,000 DBS surgeries have been performed around the world, many for the nervous system disorder.
In recent years, it's been explored as a treatment for a range of other diseases. At Sunnybrook, clinical trials are underway exploring DBS for use in disorders like post-traumatic stress disorder, obsessive-compulsive disorder, major depressive disorder, and alcohol use disorder.
What changes is the part of the brain being targeted, says Dr Nir Lipsman, the trial lead investigator and the neurosurgeon who performed Dr Plummer's surgery.

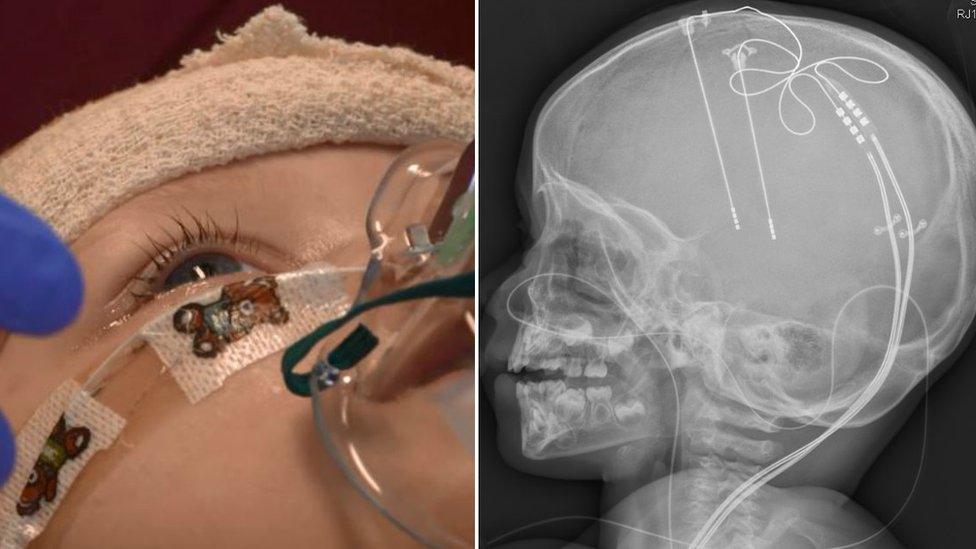
Frank Plummer was awake during the surgery
"[For] things like Parkinson's disease we target motor circuits in the brain, in addiction, alcohol use disorder, we're targeting reward, pleasure circuits of the brain," he says.
DBS treatment involves implanting an electrical device directly into a patient's brain to stimulate circuits where there is abnormal activity , or dysfunctional "wiring", and help reset them. DBS is frequently described as a type of "pacemaker" for the brain.
Electrodes are inserted into a targeted region of the brain to recalibrate activity in that area using electrical impulses - controlled by a pacemaker-like device placed under the skin of the patient's chest - and ease cravings.
Dr Plummer was the trial's first patient and underwent the experimental surgery just over a year ago. A total of six people are expected to eventually participate - all with a history of chronic alcohol use disorder proven resistant to other types of treatment.
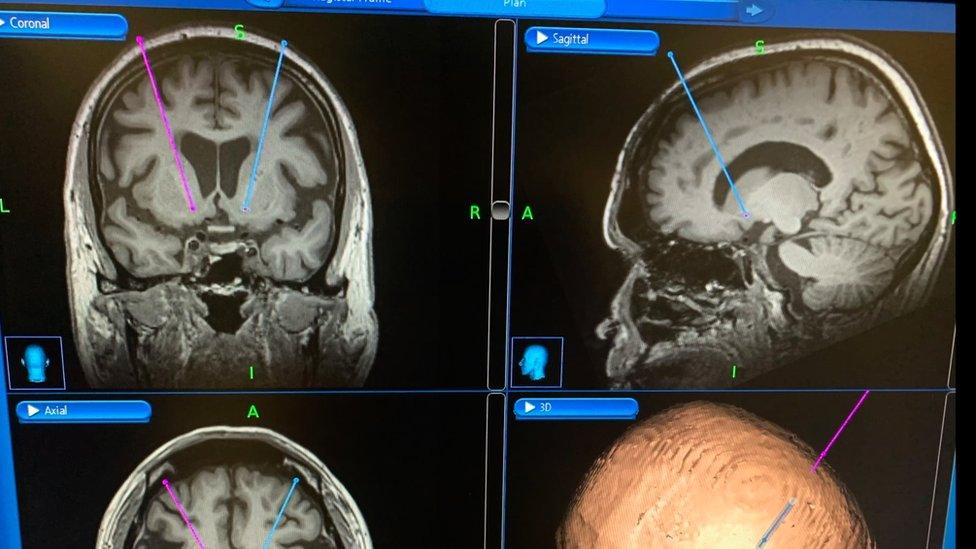
The DBS surgery performed on Frank Plummer targets the brain's nucleus accumbens, or pleasure centre
Patients are awake for the surgery.
Dr Plummer says the worst part of the procedure were the noise and vibrations when surgeons drilled into his skull in order to implant the electrodes.
"It was a large drill that drills about a 25 cent piece out of your skull on both sides - that wasn't painful but it was annoying," he says.
The brain pleasure centres being targeted in this study - the nucleus accumbens - is also involved in mood, anxiety and depression.
That factor is potentially key since many addiction disorders frequently coexist with mood disorders, the neurosurgeon says.
The surgeon says Dr Plummer has seen an improvement in both his cravings and his mood.
In those who've had the surgery, "we are seeing some signs, some early signs that we are having an impact on those kind of behaviours and those kind of measures that we want to influence", says Dr Lipsman.
The surgeons hope the study will shift some of the stigma around addiction disorders. Addictions are still often seen as a weakness or a failure of willpower, which can prevent people seeking treatment.
"We need to change the way we view addiction, change the way we view alcohol use disorder as a condition in its advanced stages, in the treatment resistant stages as being driven by circuits in the brain that are not functioning properly," he says.
But he cautions the research is in early stages - and that it's not a silver bullet.

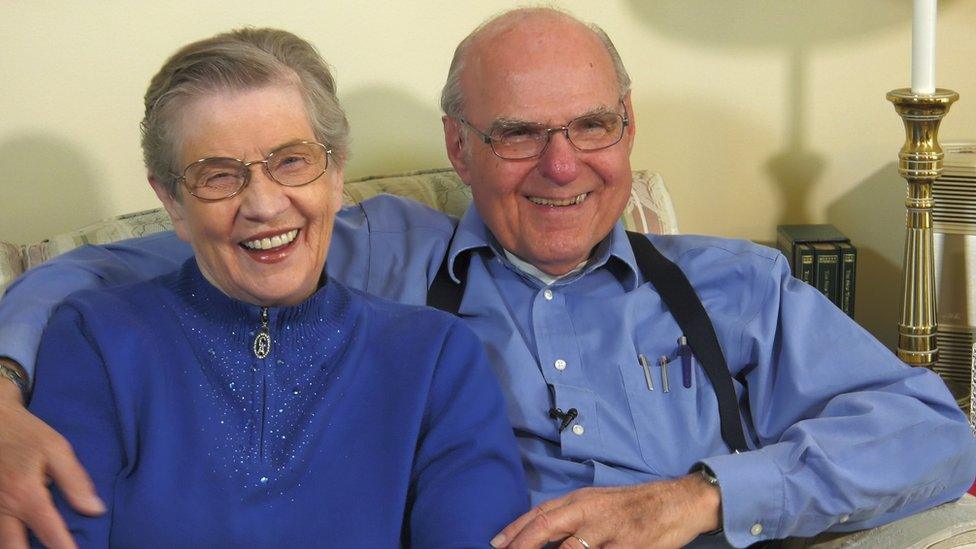
Frank Plummer, seen with his wife Jo, says he has rediscovered life since the surgery
"It's not just put in the implant, say goodbye and you're done," he says. Patients should still continue their conventional treatment for their alcohol addictions, like therapy or rehab programmes.
"It's really about viewing this as part of a larger strategy to treat what is an incredibly complex and challenging condition."
Any results from DBS are not instantaneous - it can take weeks to feel a change. For Dr Plummer, after a little while, "life just became so much better, so much richer."
"I suddenly decided that I wanted to write a book about my experiences as a scientist, and experiences living in Kenya," he says.
He's back to getting up early, writes daily and has returned to HIV research with the hopes of developing a vaccine for the disease.
He drinks occasionally but says he doesn't have the same compulsion or the physical dependency as before.
"Life is on the table again," he says.
- Published22 March 2016

- Published30 January 2018
- Published11 July 2019