What happens when you leave intensive care?
- Published
Being admitted to intensive care is a fraught time for everyone involved, but for some the "nightmare" only begins when they leave hospital.
A study of about 300 people who had been in intensive care in the UK suggests three quarters of them experienced moderate or severe pain 12 months after being discharged and 44% were significantly anxious or depressed.
You have been sharing your post-intensive care experiences:
"I sat down on the bed and literally sobbed"
Andrea Gordon cared for her husband Malcolm at their home in Bilborough, Nottingham, after his stroke in 2009.

Andrea Gordon was determined she would not let her husband Malcolm go into a home following a stroke
Mrs Gordon said: "I was told three times that my husband would not make it to see the next day. I said, "Doctor, you know your medicine, but I know my husband. He wouldn't dare leave me behind, he knows I would kill him for that."
Mr Gordon, who was 62 at the time, was kept in intensive care for three and a half weeks before being transferred to a normal ward and then being allowed to go home.
Having steeled herself to face the worst in hospital, it wasn't until her husband came home that Mrs Gordon finally broke down.
She said: "I'm riddled with arthritis and Malcolm needed lifting everywhere because he had been bedridden for a month. He was paralysed down one side and had to be hoisted about.
"They brought him home in an ambulance, gave me the hoist and I was left to do it all by myself. I had no idea how to work the hoist and I couldn't manage it on my own. I sat down on the bed and literally sobbed.
"Just when my husband needed me most, when he was depending on me, I wasn't able to look after him. I felt terrible."
Mrs Gordon said she was "told nothing" and taught herself how to care for him but looking back she said: "I could accept he had had a stroke, I just didn't know how to deal with it.
"For two and a half months I couldn't leave him on his own. I did everything for him. But then I had to have help because I had become very disabled myself. I went downhill quickly."

Mrs Gordon became ill while looking after her husband without any help but said they had persevered and have now come through the worst of it
Mrs Gordon is due to have an operation on her shoulder which she said she injured through repeatedly lifting her husband while they were waiting for home support.
The couple have since been offered a "wonderful" care package of home help for a couple of hours a day and at the weekend but the initial support when Mr Gordon left hospital "just wasn't there."
"There's no-one to guide you"
Terry Foster, an air conditioning sales rep of 30 years, from Merseyside, suffered depression following a 19-day stay in intensive care in 2011. He had been undergoing chemotherapy for lymphoma when he caught an infection. He had also recently lost his job and had just become a father for the first time.
"After the intensive care, I had a meeting with a palliative nurse who made arrangements for me to be sent home to die. Most people thought I only had a 50-50 chance of surviving.

Terry Foster was sacked for having cancer, had depression after surgery and was "sent home to die"
"When I left the hospital I had a physio once a week who taught me how to walk again. I also had someone from a local agency come and wash me in the morning but that was it.
"Looking back on it now, I am ever so grateful to the doctors who saved my life but I think I must have been very depressed. For instance I had to convince myself that both my socks matched when I got up in the morning otherwise I thought that was the day I was going to die.
"My daughter was born two days before I was released from hospital and we came home on the same day. The intensive care staff did what they needed to but then they just moved on to the next patient. There was no real follow-up system and what there was, was a complete and utter mess.
"A wheelchair was ordered for me because I couldn't walk, not even to go to the toilet, but by the time it arrived months later, I was already walking. I had only wanted to borrow it but the system wouldn't let me give it back even though I didn't need it.
"I had three home visits by three different health visitors but none of them knew the others had been, it was so disjointed.
"It was only through a Macmillan group I had joined that I was referred to a psychologist for my depression and anger. The psychologist I saw was the person I was actually meant to see after leaving hospital, but I guess I just fell through the cracks.
"He said he had no idea that I was meant to see him but that someone who had been through my experience in intensive care should have automatically been referred to him from the hospital.
"It was really a case of hunting down information for yourself. There's no-one to guide you. It would be horrific if you were foreign or elderly and confused. There isn't a book you can read or even a website that you can go to for all the information that tells you where to get help or what you're entitled to."
"Nothing beats having a face-to-face conversation with a professional"
Ernie Hayes, from Chester in Cheshire, said his excellent after-care treatment helped him to recover quickly from the trauma of intensive care following a heart attack in 2007 aged 55.
Ernie Hayes was visited by a GP every week until she was satisfied he was coping well
"I was 55 when I had my second heart attack six years ago. I was rushed into the intensive care unit and stayed there for about a week, I was transferred to the normal ward for a week and then came home.
"I was told before I left the hospital that a GP would come to visit me at home.
"I was at home that first week when a GP came to visit me and she came to visit every week for many months until she was confident that I was on the right medication and everything was under control. I'm a reasonably intelligent person and can look things up on the internet and teach myself about my condition but nothing beats having a face-to-face conversation with a professional.
"It was so reassuring to have a doctor come and see me and to take my pulse and give me a check-up. I felt that if I ever had any problems I would be able to raise them with her and contact her.
"It was so important for my wife too. It just gave her peace of mind, instead of worrying about me. When you are seriously ill, lying in bed, it is as terrible on the spouse as it is for the patient.
"But the GP came to the house and talked things through with both of us so that she could understand my condition and my progress. The after-care treatment was excellent.
"I then had a successful double by-pass in August and quickly became stable and was able to go to see the GP myself, for follow-ups. I had physio appointments and regular outpatient check-ups at three months, six months and a year."
"In hospital you're looked after almost to the point of being loved"
Richard Brooks, a 47-year-old car salesman from Bristol, had a heart attack 12 months ago and was kept in ICU for three weeks.
"I was allowed to walk out of the hospital in a bit of a daze while I was still having hallucinations from all the medication. Luckily my wife collected me 20 minutes later.

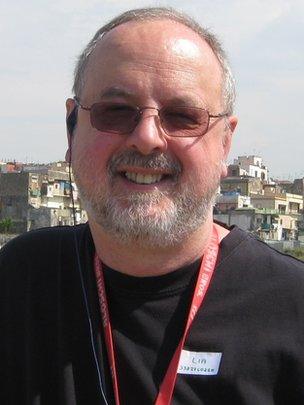
After his release from hospital Richard Brooks said he went "off the radar"
"I couldn't go to the toilet on my own, I couldn't wash on my own. I was reliant on my wife for everything.
"I didn't even get a phone call from anybody at the hospital to see how I was coping.
"When you are in hospital you are looked after almost to the point of being loved, it feels like. The care and attention of the medical staff - I really can't fault them. What happens after the hospital treatment though, seems to be a gaping gap.
"I think there was a delay in my paperwork catching up with me after being discharged, so it was about four weeks before I was enrolled on a rehabilitation programme.
"Once I was enrolled I joined a cardiac group for people in a similar position to me, it works on confidence building and was the start of the road to recovery. The classes were excellent.
"I went back to work after six months but I had to claim benefits. I was sofa-bound and there was no support whatsoever.
"The NHS is a first-class service dedicated to getting people better but I just went off the radar between coming out of hospital and before starting the classes."
Interviews by Sitala Peek
- Published28 May 2013