Rules for babies 'from three people'
- Published
.jpg)
The rules for creating babies from three people - which state only two would be classed as parents - have been announced by the UK government.
The fertility technique uses material from the mother, father and a donor woman to prevent deadly diseases.
MPs will soon vote on whether to make the UK the first country in the world to legalise the procedure.
Opponents say it is unethical to make babies with DNA from three people and that it represents a "slippery slope" .
The UK scientists that have led the research hope to offer the procedure next year.
Some families have lost up to seven children to "mitochondrial diseases" that leave the body with insufficient energy to function.
Mitochondria are the microscopic power stations in nearly every cell of the body.
Defective mitochondria are passed only from mother to child so scientists in the UK have pioneered therapies that use functioning mitochondria from a donor woman.
However, mitochondria have a tiny amount of their own DNA so any resulting child would have genetic information from three people.

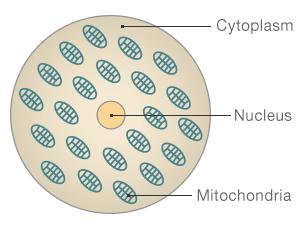
The structure of a cell
Nucleus: Where the majority of our DNA is held, which contains the genetic instructions for building and running the human body
Mitochondria: Often described as the cells' power stations, these convert energy into a form cells can use. They also contain 0.1% of the total number of genes in a person.
Cytoplasm: The jelly like substance that contains the nucleus and mitochondria

The regulations, external put before Parliament state:
The fertility regulator must assess each case for a significant risk of disability or serious illness
Fertility clinics would need a new licence to offer the technique
The woman donating her egg would not be related to the child
Any child born would have no right to information about the donor
In practice it means that only the most severely affected women - perhaps 10 cases per year - would go ahead.
And doctors in Newcastle, where the technique has been pioneered, would initially be the centre offering it.
The regulations will remain in draft form until they are voted on by Parliament and are signed off by ministers.
This is expected to take place before the general election in May 2015.
Public Health Minister Jane Ellison said: "The government considers that the time is now right to give Parliament the opportunity to consider and vote on these regulations."
Delight
Prof Doug Turnbull, from Newcastle University, told BBC News: "I'm delighted that it's being moved forward to the next stage. It's a long process but it's great news.
"We want to apply for a licence next year and hope to do it [the procedure] in 2015."
A scientific review by the fertility The Human Fertilisation and Embryology Authority said there was no evidence that it would be unsafe, but called for final checks, external.

Deadly

Baby Jessica was born with Leigh's disease, a type of mitochondrial disease, and she has to be fed through a tube.
One in every 6,500 babies has severe mitochondrial disease.
"They did warn us she may not reach her toddler years," her mother Victoria Holliday said.
She and partner Keith Newell want more children but are unwilling to risk another child suffering in the same way as Jessica.
"It's not fair that if there's a scientific technique out there that could stop this happening in the future that we're not using it," Victoria said.

Dr David King, from the the campaign group Human Genetics Alert, said: "This is hi-tech medicine at its worst and most unnecessary.
"Medical researchers are crossing the crucial ethical line that will open the door to designer babies based on scientific misinformation and ignoring majority public opposition.
"There are already safe and reliable ways to avoid these conditions, so why put the child's health at risk purely so that mothers can be genetically related to them?"
How is it done?
Two separate techniques are being devised, but they both share the same common principle - take the DNA from the parents and combine it with healthy mitochondria from a female donor.
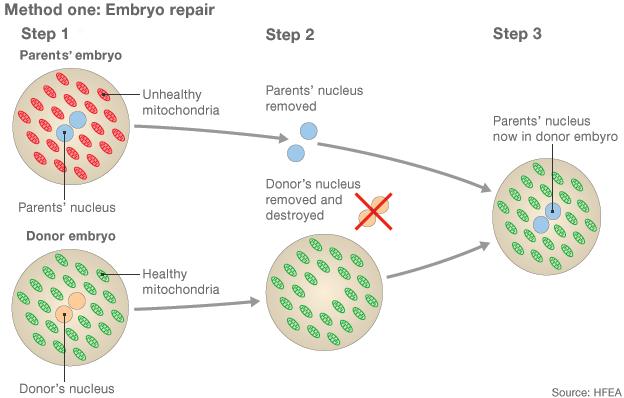
1) Two eggs are fertilised with sperm, creating an embryo from the intended parents and another from the donors 2) The pronuclei, which contain genetic information, are removed from both embryos but only the parents' are kept 3) A healthy embryo is created by adding the parents' pronuclei to the donor embryo, which is finally implanted into the womb
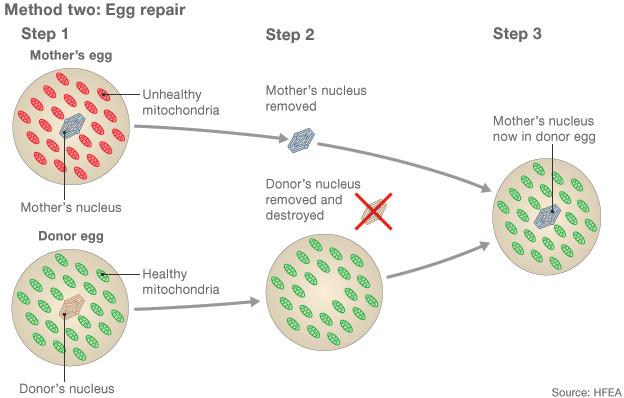
1) Eggs from a mother with damaged mitochondria and a donor with healthy mitochondria are collected 2) The majority of the genetic material is removed from both eggs 3) The mother's genetic material is inserted into the donor egg, which can be fertilised by sperm.
The pronuclear transfer method involves fertilising two eggs and moving the combined parents' DNA into the fertilised donor egg.
Spindle transfer is the other way round. The mother's DNA is moved into the donor egg, which is then fertilised.
It is unclear whether one method is safer or more effective than the other.
However, the team at Newcastle are at a more advanced stage with pronuclear transfer.
- Published3 February 2015
.jpg)
- Published17 December 2014

- Published3 June 2014

- Published28 June 2013

- Published1 September 2014